Comparison of the diagnostic performance of the modified Korean Thyroid Imaging Reporting and Data System for thyroid malignancy with three international guidelines
Article information
Abstract
Purpose
This study compared the diagnostic performance of the modified Korean Thyroid Imaging Reporting and Data System (K-TIRADS) for thyroid malignancy with three international guidelines.
Methods
From June to September 2015, 5,708 thyroid nodules (≥1.0 cm) in 5,081 consecutive patients who underwent thyroid ultrasound (US) at 26 institutions were evaluated. The US features of the thyroid nodules were retrospectively reviewed and classified according to all four guidelines. In the modified K-TIRADS, the biopsy size threshold was changed to 2.0 cm for K-TIRADS 3 and 1.0 or 1.5 cm for K-TIRADS 4 (K-TIRADS1.0cm and K-TIRADS1.5cm, respectively). We compared the diagnostic performance and unnecessary fine-needle aspiration biopsy (FNAB) rates for thyroid malignancy between the modified K-TIRADS and three international guidelines.
Results
Of the 5,708 thyroid nodules, 4,597 (80.5%) were benign and 1,111 (19.5%) were malignant. The overall sensitivity was highest for the modified K-TIRADS1.0cm (91.0%), followed by the European (EU)-TIRADS (84.6%), American Association of Clinical Endocrinologists/American College of Endocrinology/Associazione Medici Endocrinologi (AACE/ACE/AME) (80.5%), American College of Radiology (ACR)-TIRADS (76.1%), and modified K-TIRADS1.5cm (76.1%). For large nodules (>2.0 cm), the sensitivity increased to 98.0% in both the modified K-TIRADS1.0cm and K-TIRADS1.5cm. For small nodules (≤2.0 cm), the unnecessary FNAB rate was lowest with the modified K-TIRADS1.5cm (17.6%), followed by the ACR-TIRADS (18.6%), AACE/ACE/AME (19.3%), EU-TIRADS (28.1%), and modified K-TIRADS1.0cm (31.2%).
Conclusion
The modified K-TIRADS1.5cm can reduce the unnecessary FNAB rate for small nodules (1.0-2.0 cm), while maintaining high sensitivity for detecting malignancies >2.0 cm.
Introduction
Ultrasonography (US) is an essential tool for assessing the risk of malignancy of thyroid nodules and deciding whether to perform fine-needle aspiration biopsy (FNAB) [1,2]. Therefore, many international societies have proposed US-based risk stratification systems (RSS) for the clinical management of thyroid nodules [1-5]. The Korean Thyroid Imaging Reporting and Data System (K-TIRADS) is a US-based RSS proposed by the Korean Society of Thyroid Radiology (KSThR) in 2016 [1]. Since its publication, many studies have compared the diagnostic performance of the K-TIRADS for thyroid malignancy to other RSS, and have reported its clinical usefulness [6-12]. As it allows intuitive and easy assessment of the US pattern of nodules, the K-TIRADS has been applied widely in clinical practice to classify nodules during real-time US examinations.
However, recent comparative studies of RSS reported that the US-based FNAB criteria of the K-TIRADS for nodules ≥1 cm had the highest sensitivity (91.7%-100%) and lowest specificity (15.4%-28.7%) for thyroid cancers, and the highest unnecessary FNAB rate for benign nodules (71.3%-84.6%) [6-9,12-15]. The diagnostic performance was similar among the different RSS at the same biopsy size threshold for the classification categories in simulation studies [8,15]. The need to modify the biopsy criteria of the K-TIRADS to reduce the unnecessary FNAB rate while maintaining high sensitivity for detecting thyroid cancer has been suggested [8,9,12,15].
Therefore, this study was performed to compare the diagnostic performance of the US-based FNAB criteria of the modified K-TIRADS for thyroid malignancy with the RSS of three international societies: the American College of Radiology (ACR)-TIRADS, European (EU)-TIRADS, and American Association of Clinical Endocrinologists/American College of Endocrinology/Associazione Medici Endocrinologi (AACE/ACE/AME).
Materials and Methods
Compliance with Ethical Standards
The institutional review boards of the 26 participating centers approved this study (AJIRB-MED-MDB-21-062). The requirement for informed consent was waived for this retrospective review.
Study Population
Patient data collected by 26 different hospitals in Korea (Thyroid Imaging Network of Korea registry, THINK) were analyzed. From June to September 2015, 22,775 consecutive patients underwent thyroid US at the 26 participating institutions. Among them, 16,679 were excluded due to the lack of a reference standard test (biopsy or surgery) (n=4,304), thyroid nodules <1.0 cm (n=12,130), or suboptimal image quality (n=245). A further 1,015 patients with 1,102 nodules were excluded due to inconclusive biopsy results. A total of 5,708 thyroid nodules (≥1 cm) in 5,081 consecutive patients were finally included in this study (4,176 women, 905 men; mean age, 53.2 years; age range, 19 to 93 years) (Fig. 1).

Flowchart showing the study population.
US, ultrasonography; FNA, fine-needle aspiration; CNB, core-needle biopsy.
Malignant nodules were diagnosed based on the histopathological results after surgery (n=947) or malignant fine-needle aspiration (FNA) or core-needle biopsy (CNB) results (n=164). Benign nodules were diagnosed based on the histopathological results after surgery (n=394), at least two benign FNA or CNB results (n=601), and one benign FNA or CNB result (n=3,602) [16-18].
US Examination and Image Analysis
All US examinations were performed with a 10-12 or 5-14 MHz linear probe. The US images were retrospectively reviewed by 1 of 17 experienced radiologists with 8-22 years of experience in performing thyroid US using an online program (AIM AiCRO, https://study.aim-aicro.com).
Prior to the commencement of this multicenter study, training sessions were held to establish a baseline consensus regarding the US criteria. The 17 radiologists evaluated images of 15 biopsy-proven masses not included in the study, and were asked to assess the US criteria during a consensus meeting, including composition, echogenicity, margin, calcification, orientation (taller-than-wide), spongiform appearance, and intracystic echogenic foci with a comet-tail artifact. In the modified K-TIRADS, nonparallel orientation was defined as the anteroposterior diameter of a nodule being longer than its transverse diameter in the transverse plane. The benign category included spongiform or partially cystic nodules with intracystic echogenic foci with comet-tail artifact regardless of suspicious US features. All of the reviewers, who were blind to the FNAB results and final diagnoses, then assessed the US features of the thyroid nodules [3-5]. However, extrathyroidal extension status was not evaluated in this study due to a lack of standardized US criteria. An isolated macrocalcification was defined as an entirely calcified nodule with posterior acoustic shadowing, in which no soft tissue component was identified due to dark shadows on the US image [19-21]. Such nodules were classified as "intermediate suspicion" based on the modified K-TIRADS, "moderate suspicion" (4 points) based on the ACR-TIRADS, and "unclassified" based on the other RSS [1,3-5].
Biopsy Size Thresholds for the Modified K-TIRADS and Other RSS
The size threshold for biopsy was increased from 1.5 cm to 2.0 cm for low-suspicion (K-TIRADS 3) nodules in the modified K-TIRADS. The size threshold for biopsy was subdivided into 1.0 and 1.5 cm for K-TIRADS 4 (K-TIRADS1.0cm and K-TIRADS1.5cm, respectively). The biopsy size thresholds in the RSS are shown in the Supplementary Table 1. Nodules classified as low-risk based on the AACE/ACE/AME guidelines, not suspicious (TR2) or benign (TR1) based on the ACR-TIRADS, or benign based on the EU-TIRADS and modified K-TIRADS were not indicated for biopsy in this study.
Statistical Analysis
The nodules were classified according to the categories defined by the different RSS, by one radiologist (D.G.N.) with 22 years of experience in performing thyroid US and interventional procedures (Supplementary Table 1). The malignancy risk for each RSS category was calculated as a percentage. The associations between all categories and the final diagnoses were evaluated using the linear-by-linear association test.
Thyroid nodules were classified into two groups: nodules in which US-guided FNAB was not indicated and nodules in which US-guided FNAB was indicated based on the criteria of each RSS (i.e., US features and nodule size). The performance of the US-based FNAB criteria of each RSS for diagnosing thyroid cancer was evaluated based on the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy, and compared using the generalized estimating equation (GEE) method.
The potentially unnecessary FNAB rate was calculated according to the number of benign nodules among FNAB-required nodules in the total of thyroid nodules, and the number of benign nodules among FNAB-required nodules in the total of benign thyroid nodules. These values were calculated as percentages, and the results were compared among the guidelines using the GEE method. Statistical analyses were performed using SPSS for Windows version 23.0) (IBM Corp., Armonk, NY, USA) and SAS for Windows version 9.2 (SAS Institute Inc., Cary, NC, USA). In all analyses, P<0.05 was taken to indicate statistical significance.
Results
Of the 5,708 thyroid nodules, 4,597 (80.5%) were diagnosed as benign and 1,111 (19.5%) as malignant. The 1,111 malignant nodules included 1,011 papillary thyroid carcinomas (91.0%) and 62 follicular carcinomas (5.6%). The mean size of the nodules was 20.7±10.8 mm (range, 10 to 100 mm). There were 3,576 (62.6%) small nodules (1-2 cm) and 2,132 (37.4%) large (>2 cm) nodules. The malignancy rate was significantly higher in small tumors (1-2 cm) than in large tumors (>2 cm) (22.7% [810/3,576] vs. 14.1% [301/2,132], respectively; P<0.001).
Malignancy Risk by Category in the Different RSS
Table 1 lists the malignancy risk for each category in the different RSS. The malignancy probability was higher in the higher risk categories of all guidelines (P<0.001). Overall, 1.0% (59 of 5,708) of nodules were unclassified according to the AACE/ACE/AME and EU-TIRADS; however, 33.9% (20 of 59) of those were actually malignant.
Diagnostic Performance of the Modified K-TIRADS and Other RSS
Table 2 shows the diagnostic performance of the different RSS for thyroid cancer. The sensitivity and negative predictive value were highest for the modified K-TIRADS1.0cm (91.0% and 94.8%, respectively), followed by the EU-TIRADS (84.6% and 91.4%, respectively), AACE/ACE/AME (80.5% and 91.1%, respectively), ACR-TIRADS (76.1% and 91.4%, respectively), and K-TIRADS1.5cm (76.1% and 89.7%, respectively).
The modified K-TIRADS1.0cm had significantly higher diagnostic sensitivity than the AACE/ACE/AME, ACR-TIRADS, and EU-TIRADS (all P<0.001), while it showed lower specificity than the AACE/ACE/AME and ACR-TIRADS (both P<0.001) and similar specificity to the EU-TIRADS (P=0.492). The modified K-TIRADS1.5cm had lower diagnostic sensitivity than the AACE/ACE/AME and EU-TIRADS (both P<0.001), and comparable sensitivity to the ACR-TIRADS (P=0.923). It also showed higher specificity than the AACE/ACE/AME and EUTIRADS (both P<0.001).
When applying the FNAB criteria to large nodules (>2.0 cm), the sensitivity and negative predictive values increased to 89.7%-99.7% and 96.0%-97.8%, respectively. Both the modified K-TIRADS1.0cm and K-TIRADS1.5cm had high diagnostic sensitivity (98.0%) and negative predictive values (96.6%), respectively. The modified K-TIRADS1.5cm had higher diagnostic sensitivity but lower specificity than the ACR-TIRADS (98.3% and 89.7%, respectively, P<0.001; and 9.4% and 40.4%, respectively, P<0.001).
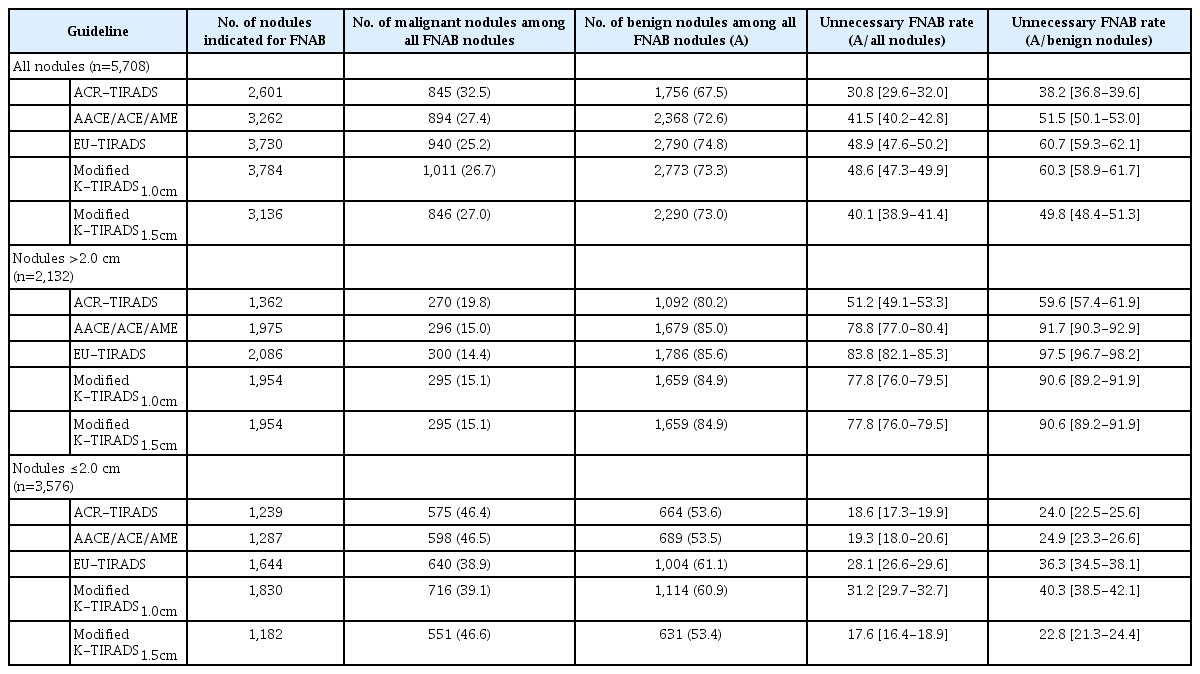
Unnecessary FNAB Rates for the Modified K-TIRADS and Other RSS
Among the RSS, the unnecessary FNAB rates for all nodules and benign nodules were lowest with the ACR-TIRADS (30.8% and 38.2%, respectively) followed by the modified K-TIRADS1.5cm (40.1% and 49.8%, respectively), AACE/ACE/AME (41.5% and 51.5%, respectively), modified K-TIRADS1.0cm (48.6% and 60.3%, respectively), and EU-TIRADS (48.9% and 60.7%, respectively) (Table 3). The modified K-TIRADS1.5cm had significantly lower unnecessary FNAB rates for all nodules than the AACE/ACE/AME, EU-TIRADS, and modified K-TRADS1.0cm (all P<0.001), but higher unnecessary FNAB rates than the ACR-TIRADS (P<0.001).
When applying the FNAB criteria to small nodules (≤2.0 cm), the unnecessary FNAB rate was lowest with the modified K-TIRADS1.5cm (17.6% and 22.8%, respectively), followed by the ACR-TIRADS (18.6% and 24.0%, respectively), AACE/ACE/AME (19.3% and 24.9%, respectively), EU-TIRADS (28.1% and 36.3%, respectively), and modified K-TIRADS1.0cm (31.2% and 40.3%, respectively). The modified K-TIRADS1.5cm had significantly lower unnecessary FNAB rates than all the other RSS (all P<0.05).
Discussion
Our study demonstrated the clinical utility of the modified K-TIRADS. The modified K-TIRADS1.5cm significantly reduced the unnecessary FNAB rates compared to the AACE/ACE/AME and EU-TIRADS in all nodules, while maintaining high sensitivity for detecting malignancy in >2.0 cm nodules (up to 98.0%). Compared to the ACR-TIRADS, it had a significantly lower unnecessary FNAB rate for small nodules (≤2.0 cm), but higher diagnostic sensitivity for detecting malignancy in nodules >2.0 cm. Although the modified K-TIRADS1.0cm increased the diagnostic sensitivity for detecting small malignancies, it should be used only after careful consideration of the risks and benefits to the individual patient.
US-based RSS has an essential role in predicting the malignancy risk of thyroid nodules and the decision to perform FNAB [1,2]. However, the sensitivity and specificity of US-based RSS for detecting thyroid cancers remain controversial. As most patients with low-risk small thyroid cancers have an excellent prognosis and low likelihood of mortality, it is also important to reduce overdiagnosis and the harm caused by overtreatment [22]. US-based RSS is expected to reduce the unnecessary FNAB rate while also maintaining appropriate sensitivity for detecting thyroid cancer. Many studies have suggested that increasing sensitivity should be the focus, regardless of the rate of unnecessary FNAB of large nodules (>2 cm), considering the higher risk of aggressive behavior in large cancers. On the other hand, reducing unnecessary FNAB for small nodules (1-2 cm) is important, given the slow growth rate of small cancers [9]. In simulation studies, when the biopsy size threshold for K-TIRADS 3 increased from 1.5 to 2 cm, there was a decrease (14.1%-16.2%) in the unnecessary FNAB rate of benign nodules, and a minimal decrease (1%-1.9%) in the sensitivity (91.6%-94.7%) for thyroid cancer, compared to the original K-TIRADS (sensitivity, 93.5%-95.7%) [8,15]. When the biopsy size threshold was increased from 1.0 to 1.5 cm for K-TIRADS 4, there was a substantial decrease (27%-28.9%) in the unnecessary FNAB rate of benign nodules and a further significant decrease (15%-27.1%) in the sensitivity (66.4%-80.7%) for thyroid cancer [8,15]. Based on these results, it was planned to modify the K-TIRADS biopsy size threshold to 2.0 cm for K-TIRADS 3 and 1.0 or 1.5 cm for K-TIRADS 4 in this study.
The modified K-TIRADS1.5cm reduced the unnecessary FNAB rate to 17.6% in small nodules (≤2.0 cm). This was significantly lower than the rate for the AACE/ACE/AME, EU-TIRADS, and ACR-TIRADS (18.6%-28.1%). Moreover, it maintained high sensitivity (up to 98.0%) for detecting large cancers (>2.0 cm). Compared to the ACR-TIRADS, the modified K-TIRADS1.5cm had a higher unnecessary FNAB rate (40.1% and 30.8%, respectively) for all nodules, a lower unnecessary FNAB rate (17.6% and 18.6%, respectively) for small nodules (≤2.0 cm), and significantly higher sensitivity for detecting large cancers (98.0% and 89.7%, respectively). The modified K-TIRADS1.0cm had a diagnostic sensitivity up to 88.4% for small cancers, but the unnecessary FNAB rate was significantly higher compared to the ACR-TIRADS and AACD/ACE/AME guidelines. Therefore, it is suggested that the modified K-TIRADS1.0cm be applied only after careful consideration of clinical factors, family history, and US features.
This study had several limitations. First, it only included thyroid nodules that had undergone US-guided FNAB, which is usually performed in thyroid nodules with suspicious US features, or in the largest nodule if no suspicious US features are detected; this may have led to selection bias. Second, the final diagnoses of benign nodules were based on the cytopathological results and surgical histological findings, which may have resulted in false-negative or false-positive results. Third, this study included a large proportion of papillary thyroid carcinomas. If the proportion of follicular cancers increase, the diagnostic performance may be changed.
In conclusion, the modified K-TIRADS1.5cm reduced the unnecessary FNAB rates in all nodules compared to the AACE/ACE/AME and EU-TIRADS, while maintaining high sensitivity for detecting malignancies >2.0 cm. In particular, it showed higher sensitivity for detecting malignancies >2.0 cm, but a lower unnecessary FNAB rate for small nodules (1.0-2.0 cm) than the ACR-TIRADS.
Notes
Author Contributions
Conceptualization: Ha EJ, Shin JH, Na DG, Jung SL, Paik W. Data acquisition: Ha EJ, Shin JH, Na DG, Jung SL, Lee YH, Paik W, Hong MJ, Kim YK, Lee CY. Data analysis or interpretation: Ha EJ, Na DG. Drafting of the manuscript: Ha EJ. Critical revision of the manuscript: Shin JH, Na DG, Jung SL, Lee YH, Paik W, Hong MJ, Kim YK, Lee CY. Approval of the final version of the manuscript: all authors.
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by a Research Fund of the Korean Society of Ultrasound in Medicine for 2021, by the Medical Research Promotion Program through the GangNeung Asan Hospital funded by the Asan Foundation (2018-C03), and by a research fund from the Korean Society of Radiology through Radiology Imaging Network of Korea for Clinical Research (RINK-CR). We thank Dr. Ji Eun Shin (Department of Radiology, CHA Gangnam Medical Center, College of Medicine, Cha University), Dr. Younghee Yim (Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine), Dr. Nami Choi (Department of Radiology, Konkuk University Medical Center, Konkuk University Scool of Medicine), Dr. Hwa Seon Shin (Department of Radiology, Gyeongsang National University Hospital), Dr. Sung-Hye You (Department of Radiology, Korea University Anam Hospital, Korea University Hospital), Dr. Beomsu Kim (Department of Radiology, Kosin University Gaspel Hospital), Dr. Jin Yong Sung (Department of Radiology, Thyroid Center, Daerim St. Mary’s Hospital), Dr. Hyun Jeong Kim (Department of Radiology, Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea), Dr. Dae Bong Kim (Department of Radiology, Dongguk University Ilsan Hospital), Dr. Ji-hoon Kim (Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine), Dr. Sun-Won Park (Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine; Department of Radiology, Seoul Metropolitan Government Seoul National University Boramae Medical Center), Dr. Ji Ye Lee (Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine), Dr. Hyun Kyung Lim (Department of Radiology, Soonchunhyang University Seoul Hospital), Dr. Ra Gyoung Yoon (Department of Radiology, Nowon Eulji Medical Center, Eulji University), Dr. Yoo Jin Lee (Department of Radiology, Busan Paik Hospital, Inje University College of Medicine), Dr. Joon Hyung Lee (Department of Radiology, Inje University Haeundae Paik Hospital), Dr. Hye Shin Ahn (Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine), Dr. Tae Yoon Kim (Department of Radiology, Hanyang University Guri Hospital, Hanyang University College of Medicine), Dr. JeeYoung Kim (Department of Radiology, Eunpyeong St. Mary's Hospital), Dr. Jung Hwan Baek (Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine), Dr. Young Jun Choi (Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine), and Dr. Sae Rom Chung (Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine) for their participation in data collection.
Supplementary Material
Supplementary Table 1.
Summary of US features and US-guided FNAB recommendations (https://doi.org/10.14366/usg.21056).