US features of normal parathyroid glands: a comparison with metastatic lymph nodes in thyroid cancer
Article information
Abstract
Purpose
This study aimed to determine the ultrasound (US) features of normal parathyroid glands (PTGs) and to evaluate whether normal PTGs can be differentiated from metastatic lymph nodes (LNs) in thyroid cancer.
Methods
This retrospective study included 10 normal PTGs and 95 metastatic LNs from thyroid cancer showing suspicious US features. The echogenicity, echotexture, echogenic foci (calcifications), cystic change, abnormal vascularity, size, shape, and location were retrospectively assessed and compared between normal PTGs and metastatic LNs.
Results
The echogenicity of normal PTGs was significantly different from that of metastatic LNs (P<0.001). Normal PTGs exhibited marked hyperechogenicity (100%), homogeneous echotexture (80%), focal intraglandular hypoechogenicity (20%), ovoid shape (90%), and focal cystic change in one case (10%). The echogenicity of metastatic LNs was markedly hyperechoic (0%), moderately hyperechoic (15.8%), mildly hyperechoic (53.7%), and hypoechoic (28.4%). The size and long axis/short axis ratios of normal PTGs were significantly smaller and larger than those of metastatic LNs (P<0.01 and P=0.022, respectively).
Conclusion
Marked hyperechogenicity was found only in normal PTGs, and small, ovoid, markedly hyperechoic structures in the paramedian central neck characterized normal PTGs. Normal PTGs may be differentiated from metastatic LNs in thyroid cancer.
Introduction
Ultrasonography (US) is an essential primary tool for the evaluation of nodular thyroid disease and parathyroid lesions. Many have believed that normal parathyroid glands (PTGs) are typically invisible and difficult to reliably identify on US [1-6]. The US features of normal PTGs have been rarely investigated and have not yet been established. The echogenicity of normal PTGs was considered hypoechoic [7,8] or isoechoic to hyperechoic [9,10] compared to the thyroid gland. A recent study by Xia et al. [11] reported that most of the presumed PTGs detected on intraoperative US or percutaneous US exhibited hyperechogenicity. Cohen et al. [12] also reported that the normal PTGs confirmed by tissue-washout parathyroid hormone (PTH) or autofluorescence showed homogeneously hyperechoic US features. To the best of the authors’ knowledge, only one study [12] reported the US features of six cases of biochemically confirmed normal PTGs. However, the detailed US features of normal PTGs identified by histopathological or biochemical methods remain to be elucidated. Normal PTGs may mimic metastatic lymph nodes (LNs) in patients with possible or proven thyroid cancer. This may be due to the size, shape, and overlap in the anatomical location of normal PTGs with those of metastatic LNs. Additionally, the hyperechoic US feature of normal PTGs is a suspicious feature predictive of metastatic LNs in thyroid cancer [13-16]. Distinguishing between normal PTGs and metastatic LNs on US is important to accurately provide a preoperative diagnosis of metastatic LNs and prevent unnecessary fine needle aspiration (FNA) of normal PTGs misdiagnosed as suspicious metastatic LNs in patients with possible thyroid cancer. Therefore, the aim of the present study was to determine the US features of normal PTGs, confirmed via FNA washout PTH, and evaluate whether normal PTGs could be differentiated from metastatic LNs in thyroid cancer.
Materials and Methods
Compliance with Ethical Standards
This study was performed in accordance with the Declaration of Helsinki. This human study was approved by the GangNeung Asan Hospital Institutional Review Board (2021-08-010). Due to the retrospective nature of this study, the need for informed consent was waived.
Study Population
Between March 2017 and August 2021, 118 consecutive patients with thyroid nodules underwent biopsy for 141 suspicious cervical lesions showing suspicious US features of metastatic LNs on preoperative FNA or core needle biopsy (CNB) for thyroid nodules. Twenty-one consecutive patients underwent biopsy for 32 suspicious metastatic lesions during postoperative surveillance of thyroid cancer. Therefore, during the study period, 139 consecutive patients underwent FNA for 173 suspicious metastatic lesions presenting suspicious US features of cervical metastatic LNs in thyroid cancer. A lesion was classified as suspicious for metastasis if any suspicious US feature of metastatic LNs (hyperechogenicity, calcification, cystic change, and abnormal vascularity) was identified [17]. Among 173 suspicious metastatic lesions, 21 parathyroid lesions of 21 patients (20 preoperative and one postoperative [hemithyroidectomy]) were identified by the high level of measured FNA-washout PTH (>100 pg/mL) [18-20]. Serum PTH and calcium levels were evaluated in most patients with high levels of tissue PTH.
A normal PTG was defined as a parathyroid lesion without a typical US feature of parathyroid cyst or neoplasm [8,21] in patients with normal serum PTH and calcium levels. Eleven parathyroid lesions were excluded from the 21 identified parathyroid lesions due to normocalcemic hyperparathyroidism (n=4), incidental parathyroid adenomas (n=4), incidental parathyroid cysts (n=2), and parathyroid lesions without preoperative serum PTH measurements (n=1). Thus, the final number of participants with normal PTGs was 10 (group 1; seven women and three men; mean age, 49.1 years) (Fig. 1).
During the same study period, 398 consecutive patients underwent preoperative thyroid US examinations and thyroid surgery for malignant thyroid tumors. The group of patients with metastatic LNs (group 2) only included patients with metastatic LNs that exhibited US features suspicious for metastatic LNs on preoperative thyroid US. Group 2 was used to compare the US features between normal PTGs and metastatic LNs. After a review of the electronic medical records and US reports of all patients, 351 patients without metastatic LNs showing suspicious US features on preoperative US were excluded. The exclusion criteria were as follows: (1) no metastatic LNs (n=245) in the postoperative pathology report, (2) microscopic metastatic LNs (n=66), and (3) macroscopic metastatic LNs without suspicious US features on preoperative US (n=40). Based on a retrospective level-by-level radiologic-pathologic correlation of metastatic LNs, 47 patients (37 women and 10 men; mean age, 58.8 years) with 95 metastatic LNs showing suspicious US features were finally included in the group of patients with metastatic LNs (group 2) (Fig. 1). The metastatic LNs in this study were diagnosed by both preoperative biopsy (FNA or CNB) and surgery (n=43) or by surgery alone (n=52). There was no overlap of patients between the study populations of groups 1 and 2. That is, none of the patients with normal PTGs (group 1) simultaneously had metastatic LNs and only one patient with papillary thyroid cancer in group 1 underwent thyroid surgery at the authors’ affiliated institution.
Biopsy Procedure for Suspicious Metastatic LNs
US-guided FNA was performed in one to two suspicious metastatic LNs in most patients, while CNB was selectively performed for suspicious metastatic LNs (large LNs, suspected high-grade thyroid cancer or medullary carcinoma, and suspected metastatic LNs from non-thyroid organs). Freehand technique US-guided FNA was performed using a 21- or 23-gauge needle and a 5-mL disposable syringe. The combined method of a capillary and aspiration technique was employed. SurePath (BD, Franklin Lakes, NJ, USA) liquid-based cytology was used to establish a cytopathologic diagnosis via FNA. US-guided CNB procedures were performed using a disposable 1.1-cm excursion, 18-gauge, single- or double-action spring-activated needle (Stericut [TSK, Tokyo, Japan] or Ace-cut [Create Medic, Yokohama, Japan]). The CNB needle notch was positioned within the target lesions. Strict vessel mapping along the approach route was performed using color Doppler US during the procedure to avoid vessel injury. FNA-washout thyroglobulin was routinely measured for patients with lateral neck lesions and selectively for those with central neck lesions. FNA-washout PTH measurements were selectively obtained for central neck lesions to rule out parathyroid lesions. The parathyroid lesions were suspected when the lesions showed typical US features of parathyroid cyst or parathyroid adenoma [8,19] and when well-defined, round or oval, and isoechoic to hyperechoic small lesions were observed at the anatomical location of the PTG [10,11]. The FNA needle sample was rinsed using a 23-gauge needle with 1 mL saline and was assayed for thyroglobulin and PTH levels.
Ultrasound Examinations and Image Analysis
All US examinations and biopsy procedures for the thyroid nodules and cervical LNs were performed using a 5-12 MHz linear-array transducer (EPIQ7, Philips Healthcare, Bothell, WA, USA) by two radiologists with 22 and 4 years of experience, respectively, in performing thyroid US imaging and interventions. The US images of all suspicious US features found in suspicious metastatic lesions were routinely obtained during the US examinations. The US features of normal PTGs and metastatic LNs were retrospectively assessed by an experienced radiologist (D.G.N.) blinded to the patients’ clinical histories and final diagnoses. The reviewer assessed the echogenicity, echotexture, echogenic foci (calcifications), cystic change, abnormal vascularity, size, shape, and location of the lesions. The echogenicity was categorized as marked hyperechogenicity (hyperechoic relative to the normal thyroid gland), moderate hyperechogenicity (isoechoic relative to that of the normal thyroid gland), mild hyperechogenicity (hyperechoic relative to the neck muscles and hypoechoic relative to the normal thyroid gland), and hypoechogenicity (isoechoic or hypoechoic relative to the neck muscles). In patients with diffuse thyroid disease and decreased parenchymal echogenicity, the homogenous hyperechoic echogenicity of the presumed normal thyroid gland was used as the reference structure. The echotexture of PTGs and metastatic LNs was categorized as homogeneous or heterogeneous. The homogeneous echotexture was defined as uniform echogenicity with one category of echogenicity. In contrast, heterogeneous echotexture was defined as mixed echogenicity with more than one category of echogenicity. If the lesion had a mixed pattern, echogenicity was determined using the predominant echogenicity. Echogenic foci (calcifications) were classified as punctate echogenic foci (microcalcification) (punctate [≤1 mm] hyperechoic foci with or without posterior acoustic artifacts) or large echogenic foci (large [>1 mm] hyperechoic foci with or without posterior acoustic artifact), including macrocalcification and rim calcification [16]. The presence of cystic changes was determined if any focal anechoic area was found within the lesion, or if the lesion was entirely anechoic. Abnormal vascularity was characterized by a peripheral or chaotic diffuse vascularity on color Doppler US images. The shape of the lesion was assessed using the long axis/ short axis (L/S) ratio and was categorized as round (L/S ratio ≤1.5) or ovoid (L/S ratio >1.5). The classifications of the location of lesions included the central or lateral neck. The central neck was classified as midline (prelaryngeal and pretracheal) and paramedian (superior thyroid pole, superior perithyroidal, inferior perithyroidal, inferior thyroid pole, and infrathyroidal) central neck. Whether the lesion was located at the superior or inferior thyroid pole was determined when the epicenter of the lesion was outside the thyroid gland but partially attached to the thyroid pole. The lesions located at the superior and inferior perithyroidal paramedian central neck were subcategorized as anterior, posterior, medial, or lateral according to the site of the lesion around the thyroid gland. The lateral neck was classified by the LN levels according to the eighth edition of the American Joint Committee on Cancer TNM classification system [22].
Data and Statistical Analyses
Categorical variables are reported as frequencies and percentages for each category. Continuous variables are presented as the median (interquartile range) or the mean±standard deviation, according to whether they had a parametric or nonparametric distribution, respectively. The Pearson chi-square test was used to compare the US findings between normal PTGs and metastatic LNs. The Mann–Whitney U Test was used to compare the long and short diameters for size and L/S ratios between normal PTGs and metastatic LNs. The statistical analysis was performed using SPSS version 24.0 for Windows (IBM Corp., Armonk, NY, USA). A significant difference was defined as one with a P-value <0.05.
Results
Demographic Data
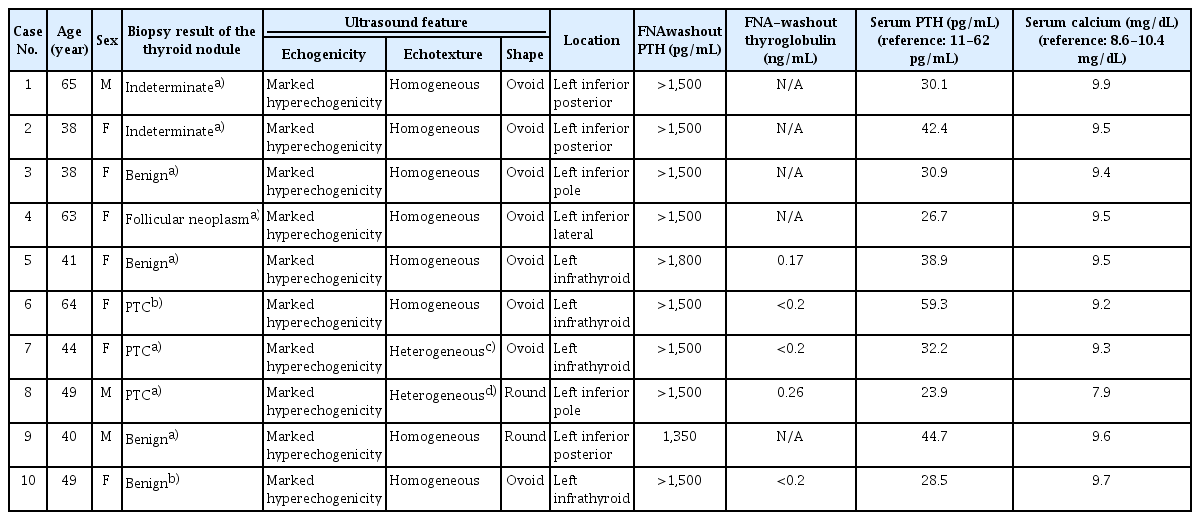
The demographic data are summarized in Table 1. There was no significant difference in sex (P=0.551) between normal PTGs and metastatic LNs, but the mean age of participants with normal PTGs was significantly younger than those with metastatic LN (P=0.049). The long and short diameters of metastatic LNs were significantly larger than those of normal PTGs (P=0.009 and P<0.001, respectively). The L/S ratios of normal PTGs were significantly larger than those of metastatic LNs (P=0.022). In the 47 patients with metastatic LNs, the postoperative histologic types of thyroid cancers were papillary carcinoma (n=44), including follicular variant papillary carcinoma (n=4), follicular carcinoma (n=1), medullary thyroid carcinoma (n=1), and anaplastic thyroid carcinoma (n=1).
The clinical characteristics of the 10 identified normal PTGs are summarized in Table 2. The measured FNA-washout PTH levels were very high (>1,350-1,800 pg/mL), whereas the serum PTH levels were within the normal range (23.9-59.3 pg/mL). The measured FNA-washout thyroglobulin levels were ≤0.26 ng/mL in five patients in whom FNA washout thyroglobulin was measured without contamination of thyroid tissue. The total serum calcium levels were within the normal range (7.9-9.9 mg/dL).
Comparison of US Features between Normal PTGs and Metastatic LNs
The US features of normal PTGs and metastatic LNs are summarized in Table 3. The echogenicity of normal PTGs was significantly different from that of metastatic LNs (P<0.001). All normal PTGs consistently showed marked hyperechogenicity, whereas marked hyperechogenicity was not found in any metastatic LNs (Figs. 2, 3). The echogenicity of 95 metastatic LNs was classified as moderately hyperechoic in 15 (15.8%), mildly hyperechoic in 51 (53.7%), hypoechoic in 27 (28.4%) LNs, and not assessable in two (2.1%) entirely calcified metastatic LNs. Mild or moderate hyperechogenicity alone without concurrent other suspicious US feature was found in 16 (16.8%) metastatic LNs with suspicious US features (Fig. 4).

Normal parathyroid gland with typical ultrasound features in the inferior posterior perithyroidal central neck in a 65-year-old male patient (case 1).
A, B. Transverse and longitudinal images show an ovoid, homogeneous, markedly hyperechoic parathyroid gland brighter than the thyroid gland at the inferior posterior margin of the left thyroid gland (arrows).

Normal parathyroid gland with typical ultrasound features in the infrathyroid paramedian central neck in a 41-year-old female patient (case 5).
A, B. Transverse and longitudinal images show an ovoid, homogeneous, markedly hyperechoic parathyroid gland in the left infrathyroid central neck (arrows).

Metastatic lymph nodes with a homogeneous moderate hyperechogenicity from infiltrative follicular variant papillary carcinoma of a 61-year-old male patient.
The transverse image shows ovoid, moderately hyperechoic lymph nodes (arrows) showing similar echogenicity to that of the thyroid gland in the right inferior posterior perithyroidal central neck (level VI). The lymph node does not show echogenic foci or a cystic change. The metastatic lymph nodes were diagnosed by surgery.
Homogeneous echotexture was found in eight of 10 normal PTGs (80%), while heterogeneous echotexture in two of 10 normal PTGs (20%). The two normal PTGs with heterogeneous echotexture showed a focal, linear, relatively hypoechoic lesion in the center of the PTG and a focal, round hypoechoic lesion with suspicion of anechoic cystic change (Fig. 5). The focal round hypoechoic lesion within the normal PTG was confirmed as a small parathyroid cyst with clear fluid by FNA. Metastatic LNs showed a lower frequency (42.1%, 40/95) of homogeneous echotexture than normal PTGs, without statistical significance (P=0.072).

Normal parathyroid glands with focal hypoechoic lesions (cases 7 and 8).
A. A longitudinal image shows an ovoid, markedly hyperechoic parathyroid gland with central linear mild hypoechogenicity (arrow) in the left infrathyroid central neck in a 44-year-old female patient. B, C. Transverse and longitudinal images show a round, markedly hyperechoic parathyroid gland with a small, round, anechoic cystic lesion with posterior acoustic enhancement (arrows) at the inferior pole of the left thyroid gland in a 49-year-old male patient. The intraglandular cystic lesion was identified as a parathyroid cyst showing clear fluid on fine needle aspiration.
Focal cystic change was found in one case (10%), and echogenic foci (calcification) or abnormal vascularity on color Doppler images was not found in any of the normal PTGs. Meanwhile, echogenic foci (calcifications) were found in 60 (63.2%) and abnormal vascularity in 29 (30.5%) of 95 metastatic LNs (P<0.001 and P=0.011, respectively) (Fig. 6). Cystic change and abnormal vascularity were more frequently found in lateral than in central metastatic LNs (P=0.042 and P=0.002, respectively). However, there were no significant differences in echogenicity, echotexture, and echogenic foci between central and lateral metastatic LNs. Eight (20%) of 10 normal PTGs demonstrated an ovoid shape. There was no significant difference in the frequency of ovoid shape between normal PTGs and metastatic LNs (P=0.821).

Metastatic lymph nodes with mild hyperechogenicity from papillary thyroid carcinomas.
A. A transverse image shows a lymph node (arrows) that is slightly hyperechoic compared to the neck muscle at the pretracheal midline central neck (level VI) in a 63-year-old female patient. The lymph node shows an ovoid shape on the longitudinal image (long axis/short axis ratio, 1.8) (not shown). It does not show echogenic foci or a cystic change. The metastatic lymph node was diagnosed by fine needle aspiration and surgery. B. A transverse image shows an ovoid, mildly hyperechoic lymph node in the left infrathyroid paramedian central neck (level VI) in a 42-year-old female patient. The lymph node shows echogenic foci (arrows). The shape was ovoid on the longitudinal image (long axis/short axis ratio, 2) (not shown). The metastatic lymph node was diagnosed by surgery.
Distribution of Normal PTGs and Metastatic LNs in the Central Neck
The distribution of normal PTGs and metastatic LNs in the central neck are summarized in Table 4. All identified normal PTGs were located in the left paramedian central neck, particularly the infrathyroid level VI area (n=4, 40.0%), inferior perithyroidal region (n=4, 40.0%; posterior 3 and lateral 1) and inferior thyroid pole (n=2, 20.0%) (Figs. 2, 3). Metastatic LNs were located in the midline (n=11, 35.5%) and paramedian region (n=20, 64.5%). Metastatic LNs found in the paramedian central neck were most frequently located in the infrathyroid level VI (n=11, 35.5%), followed by the inferior perithyroidal region (n=7, 22.6%; all posterior) and inferior pole (n=2, 6.5%).
Discussion
In this study, all normal PTGs exhibited marked hyperechogenicity, whereas no metastatic LNs showed marked hyperechogenicity. Metastatic LNs showed variable echogenicity, including hypoechogenicity and mild or moderate hyperechogenicity. Cystic change was mostly found in metastatic LNs, whereas echogenic foci (calcifications) and abnormal vascularity were exclusively found in metastatic LNs.
The present study suggests that the US pattern of a small, ovoid, homogeneous, markedly hyperechoic structure located in the paramedian central neck is a distinctive feature of normal PTGs. Normal PTGs may uncommonly show focal hypoechogenicity within the gland. In two cases of normal PTGs with focal intraglandular hypoechogenicity, the residual hyperechoic area consistently showed the same homogeneous marked hyperechogenicity as the other typical normal PTGs. A recent study [12] reported that all normal PTGs showed homogeneous hyperechogenicity in six cases. However, in their study, the echogenicity of normal PTGs was not clearly evaluated compared to that of the normal thyroid gland.
The origin of hyperechogenicity of normal PTGs may be caused by abundant stromal fat content diffusely distributed in the PTG, accounting for 35%-50% of the gland, and the stromal fat content increases with aging [23-25]. This heterogeneous glandular architecture contains numerous interfaces and may result in increased echogenicity of glandular tissue. In parathyroid adenoma and hyperplasia, the stromal fat content is displaced due to the proliferation of chief cells [26], resulting in a homogeneous architecture in the cellular proliferation area and hypoechogenicity on US [27]. An early-stage parathyroid adenoma or cyst can develop within a normal PTG, which may show focal nodular hypoechogenicity, as in one of the cases in this study (case 7). However, the identity of intraglandular linear hypoechogenicity found in the other case (case 3) is uncertain. Xia et al. [11] reported a similar finding that some presumed PTGs uncommonly showed a heterogeneous echotexture with focal hypoechogenicity inside the gland. Further investigation is needed to determine the frequency, histopathologic identity, and clinical significance of intraglandular hypoechogenicity detected in normal PTGs.
Until recently, normal PTGs were hardly detected on US [2–4]. The reason may be mainly because the US features of normal PTGs are not well recognized and small differences in echogenicity make it difficult to distinguish normal PTGs from thyroid or perithyroid adipose tissue. This may also possibly be due to the limited resolution capability of applied US equipment.
Normal PTGs may mimic metastatic LNs with suspicious US features in thyroid cancer patients. Metastatic LNs from thyroid cancer are frequently found in the central neck, and their location overlaps with that of normal PTGs. Nodal focal or diffuse hyperechogenicity is a characteristic US feature of metastatic LNs in thyroid cancer [16,28,29], and nodal hyperechogenicity may manifest without other suspicious US features in metastatic LNs. This study suggests that marked hyperechogenicity, characterized as slightly brighter echogenicity than normal thyroid echogenicity, is the characteristic and specific US feature of normal PTGs. This may differentiate normal PTGs from metastatic LNs showing suspicious US features. If a small ovoid structure located in the paramedian central neck represents homogeneous marked hyperechogenicity relative to the thyroid gland, a normal PTG is highly suggested, and the possibility of metastatic LNs may be reliably excluded. Therefore, a normal PTG should not be misdiagnosed as a suspicious LN during the preoperative evaluation of patients with possible thyroid cancer and postoperative US surveillance of thyroid cancer patients. Recognition of the characteristic US features of normal PTGs allows accurate differentiation from metastatic LNs. Furthermore, unnecessary FNA or central neck dissection during thyroid surgery may be avoided.
These results provide a basis for the potential clinical application of the preoperative localization of normal PTGs in patients undergoing thyroid surgery. An accurate preoperative localization of normal PTGs via US may help prevent possible injury of normal PTGs during thyroid surgery and might reduce postoperative hypoparathyroidism [30]. Further research is needed on the capability of advanced high-resolution US for the preoperative detection and localization of normal PTGs in a large population of patients undergoing thyroid surgery.
This study has several limitations. First, it included only a small number of normal PTGs because this retrospective study analyzed only incidentally detected normal PTGs during the study period when the US features of normal PTGs were not fully recognized. It would be very difficult to collect percutaneous US images of a large number of normal PTGs identified by a histopathological or biochemical method for research purposes. Second, selection bias inevitably existed in the group of patients with normal PTGs. Therefore, the evaluation of the frequency and distribution of normal PTGs identified in the present study was limited. Third, only one experienced radiologist retrospectively assessed the US features of normal PTGs and metastatic LNs, and the interobserver reliability was not evaluated. Fourth, this study did not compare US features of normal PTGs and metastatic LNs showing indeterminate or benign US features. However, normal PTGs will be clearly distinguished from metastatic LNs showing indeterminate or probably benign US feature, as these metastatic LNs have hypoechogenicity similar to the anterior neck muscles.
In conclusion, the US feature of a small ovoid structure with homogeneous marked hyperechogenicity is the distinctive typical feature of normal PTGs. All normal PTGs consistently showed marked hyperechogenicity, whereas no metastatic LNs showed marked hyperechogenicity. Moreover, metastatic LNs showed variable echogenicity and frequently other suspicious US features. Thus, normal PTGs may be differentiated from metastatic LNs in thyroid cancer.
Notes
Author Contributions
Conceptualization: Na DG. Data acquisition: Kim SJ, Na DG. Data analysis or interpretation: Na DG, Noh BJ. Drafting of the manuscript: Kim SJ, Na DG. Critical revision of the manuscript: Kim SJ, Na DG, Noh BJ. Approval of the final version of the manuscript: all authors.
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by the Medical Research Promotion Program through the Gangneung Asan Hospital funded by the Asan Foundation (2022II0011).
References
Article information Continued
Notes
Key point
A small, ovoid, homogeneous, markedly hyperechoic structure located in the paramedian central neck characterizes a normal parathyroid gland. All normal parathyroid glands consistently showed marked hyperechogenicity, whereas no metastatic lymph node showed marked hyperechogenicity. Normal parathyroid glands may be differentiated from metastatic lymph nodes in thyroid cancer.