AbstractCompared to the risk-oriented approach to ovarian lesions that is presented in the Ovarian- Adnexal Reporting and Data System (O-RADS) US Risk Stratification and Management System as a guideline, a lesion-oriented flowchart is more user-friendly for radiologists. In the present article, the O-RADS guideline has been depicted in the form of a single flowchart to explain how to approach ovarian lesions in an algorithmic manner. In addition to providing a practical flowchart, this pictorial article contains some images of the related ovarian lesions.
IntroductionTransvaginal ultrasonography is the first standard modality for assessing adnexal lesions [1,2]. Since the Ovarian-Adnexal Reporting and Data System (O-RADS) US Risk Stratification and Management System was published as a guideline in 2018, its use has grown among general radiologists. This guideline incorporates both common North American and European approaches and, with the same lexicon used by International Ovarian Tumor Analysis, more comprehensively covers all benign and malignant ovarian lesions [3,4]. Despite the guideline authorsŌĆÖ efforts to simplify it to the extent possible, the lack of a practical flowchart in the guideline is felt to be a shortcoming.
In comparison to the risk-oriented approach to an ovarian lesion that is noted in the abovementioned guideline, a lesion-oriented flowchart would be more user-friendly for radiologists. To date, numerous attempts have been made to simplify the content of the guideline, but none have yet fit the content into a single flowchart. Therefore, the present article aimed to summarize the findings of the guideline in the form of a flowchart to explain how to simply approach ovarian lesions in an algorithmic manner (Fig. 1). In addition to providing a practical flowchart for use by radiologists in the field of gynecology, an attempt has been made to make this article more practical by providing some images of the related ovarian lesions. All images used in this article are original and have been taken from patients who underwent imaging at Arash WomenŌĆÖs Hospital Imaging Center affiliated with Tehran University of Medical Sciences. Informed consent was obtained from all patients.
Explanation of FlowchartAccording to the O-RADS, ovarian lesions are divided into two general categories: classical and non-classical. Classical benign lesions include typical hemorrhagic cysts, endometrioma, dermoid cysts, peritoneal inclusion cysts, paraovarian cysts, and hydrosalpinx, which have typical appearances. In these cases, the size of the lesions is decisive. If their largest diameter is less than 10 cm, they are almost certainly benign and are classified into O-RADS category 2 (Fig. 2). Classical benign lesions with a diameter greater than 10 cm are deemed to have a low risk for malignancy and are marked as O-RADS category 3 (Fig. 3). Non-classical ovarian lesions are divided into solid and cystic groups. Solid lesions have smooth or irregular margins. Solid lesions with irregular margins are classified directly in O-RADS category 5. If the margin of the solid lesion is smooth, a color Doppler study is helpful. If no vascular flow (color score=1) is seen on the color Doppler examination, the lesion can be categorized as O-RADS category 3. On the other hand, if it is severely vascular (color score=4), O-RADS category 5 is considered (Fig. 4). Finally, lesions with minimal to moderate vascular flow (color scores=2, 3) are classified as O-RADS category 4.
For cystic ovarian lesions, the first step is to determine whether they are simple or not. If they are simple lesions, their size is important. Simple cystic lesions are mainly O-RADS category 2. However, if they are equal to or larger than 10 cm in size, they will have a higher risk of malignancy.
Non-simple cystic lesions may be unilocular or multilocular. Unilocular non-simple cystic lesions are classified as O-RADS category 3 if they show a smooth inner wall measuring 10 cm or more or have an irregular inner wall of any size. When encountering a unilocular non-simple cystic lesion with solid components, attention should be paid to the number of papillary projections (PPs) in it (Fig. 5). Any lesion with PPs is at an intermediate to high risk of malignancy. In multilocular ovarian lesions, the risk of malignancy is intermediate to high if there is a solid component. Nonetheless, the presence of PPs in these lesions is difficult to assess. Thus, a color Doppler examination of the lesions is required. Furthermore, if a lesion shows absent or minimal vascularity, the risk of malignancy is intermediate (Fig. 6). If it shows moderate to very strong vascular flow, however, the risk of malignancy is considered high.
An important point to keep in mind is that a vascular flow assessment is not necessary for multilocular lesions with irregular inner walls, and those lesions are at intermediate risk of malignancy (O-RADS category 4). In multilocular lesions with smooth inner walls, however, it is still recommended to assess the vascularity of the lesions. If very strong vascularity is observed, the risk of malignancy is intermediate; otherwise, the size of the lesion should be taken into account. Multilocular lesions with smooth inner walls are in O-RADS category 3 if they are smaller than 10 cm (Fig. 7) and in O-RADS category 4 if they are 10 cm or larger.
In general, any ascites or peritoneal nodule maximizes the chance of malignancy of ovarian lesions, and ovarian lesions with these two combined features are assigned to O-RADS category 5 (Fig. 8).
SummaryAs illustrated herein, a lesion-oriented approach to ovarian lesions is more useful for radiologists. As a general division, it should be determined whether ovarian lesions have solid components or not. While simple cysts are usually benign, non-simple ones are at higher risk of malignancy, especially when irregularity of the inner wall and PPs exist. The presence of solid components increases the risk of malignancy. The vascularity of the lesions is determinative of the risk of malignancy in multilocular ovarian lesions, where it is not possible to evaluate the solid component well. Paying attention to pertinent items such as ascites and peritoneal involvement is also mandatory.
NotesAuthor Contributions Conceptualization: Mohamadian A, Katouli FS. Data acquisition: Bayani L. Drafting of the manuscript: Mohamadian A. Critical revision of the manuscript: Bayani L, Katouli FS. Approval of the final version of the manuscript: all authors. AcknowledgementsThe authors would like to thank Ms. A. Keivanshekouh at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for her invaluable assistance in editing the manuscript.
References1. Kaijser J, Vandecaveye V, Deroose CM, Rockall A, ThomassinNaggara I, Bourne T, et al. Imaging techniques for the pre-surgical diagnosis of adnexal tumours. Best Pract Res Clin Obstet Gynaecol 2014;28:683ŌĆō695.
2. Meys EM, Kaijser J, Kruitwagen RF, Slangen BF, Van Calster B, Aertgeerts B, et al. Subjective assessment versus ultrasound models to diagnose ovarian cancer: a systematic review and meta-analysis. Eur J Cancer 2016;58:17ŌĆō29.
Simplified flowchart for approaching ovarian lesions based on the O-RADS US Risk Stratification and Management System.O-RADS, Ovarian-Adnexal Reporting and Data System; O, O-RADS score; CS, color score (CS1, no flow; CS2, minimal flow; CS3, moderate flow; CS4, very strong flow); PreMW, premenopausal women, PostMW, postmenopausal women; US, ultrasonography; MRI, magnetic resonance imaging; IW, inner wall; PP, papillary projections.
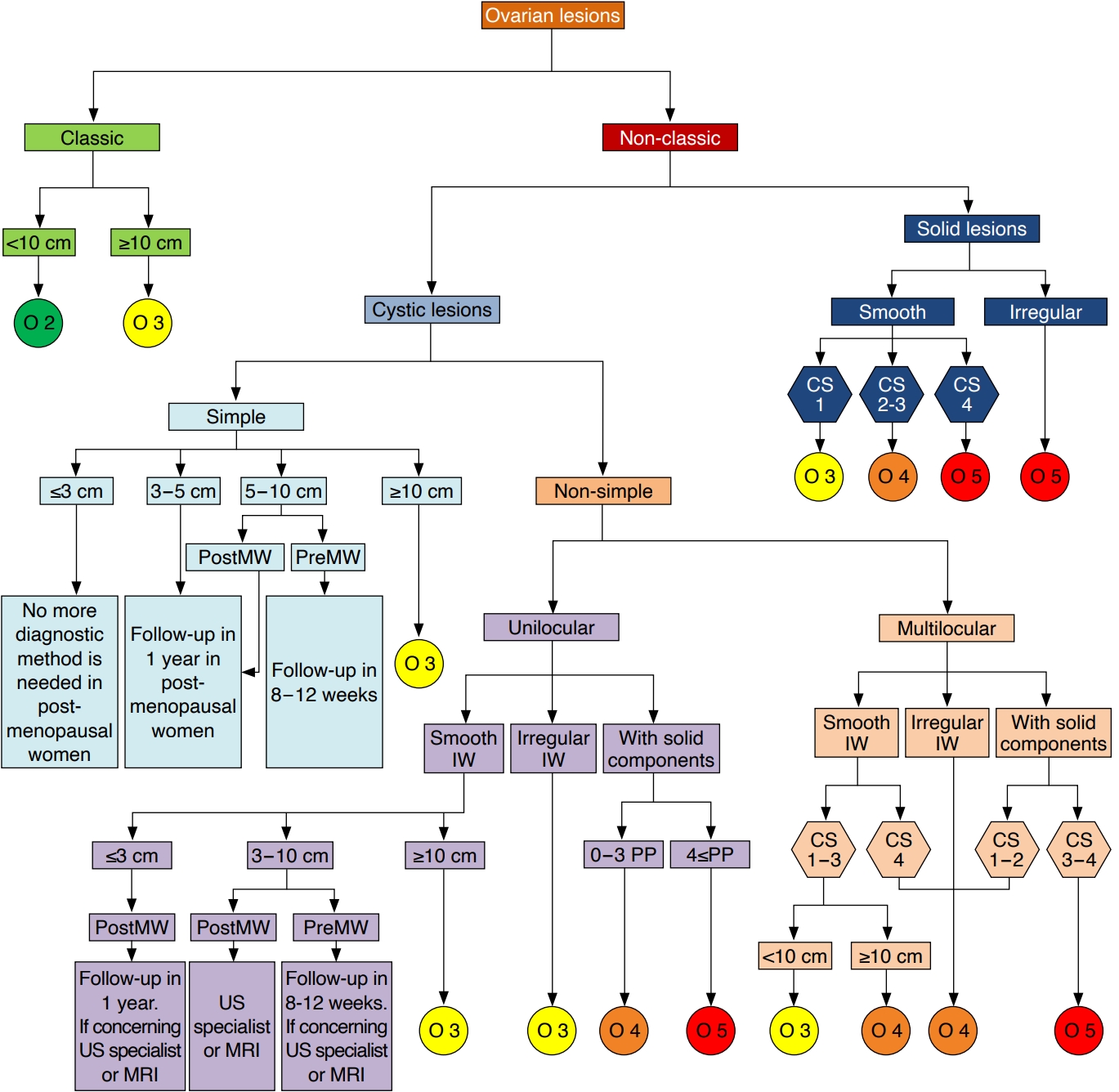 Fig.┬Ā1.Some classic benign lesions classified as O-RADS category 2.A. A cystic lesion in a 26-year-old woman with a maximum diameter of 62 mm contains homogeneous low-level echoes that are typical of endometrioma. B. A cystic lesion in a 30-year-old woman with a maximum diameter of 38 mm is depicted with fine intersecting lines depicting fibrin strands and an echogenic component with margins representing a retracting clot. C. A typical dermoid cyst is visible in a 28-year-old woman with a maximum diameter of 38 mm, containing hyperechoic lines and dots indicating hairy contents. O-RADS, Ovarian-Adnexal Reporting and Data System.
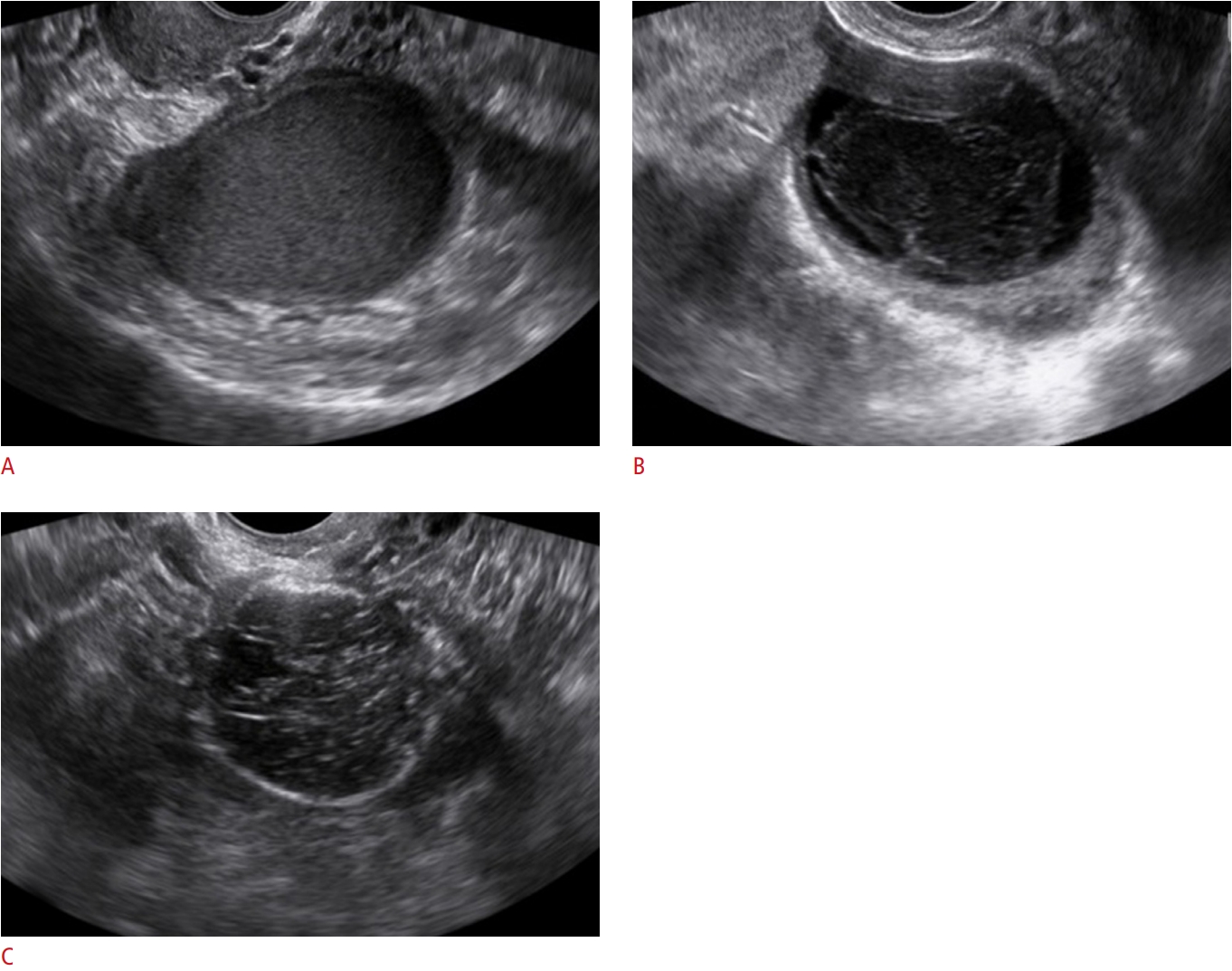 Fig.┬Ā2.Classic benign lesions classified as O-RADS category 3 due to their size.A. A cystic lesion in a 29-year-old woman with a maximum diameter of 115 mm contains homogeneous low-level echoes that are typical of endometrioma. B. A typical dermoid lesion in a 22-year-old woman with a maximum diameter of 110 mm contains a hyperechoic component with an acoustic shadow. O-RADS, Ovarian-Adnexal Reporting and Data System.
 Fig.┬Ā3.A solid lesion with a smooth outer margin classified as O-RADS category 5 due to very strong flow in color Doppler imaging.A. A solid ovarian lesion in a 53-year-old woman is depicted with a smooth outer margin. B. Very strong flow is detected in a color Doppler examination. C. Liver metastasis is present, as a hyperechoic lobulated lesion in the right lobe is notable. O-RADS, Ovarian-Adnexal Reporting and Data System.
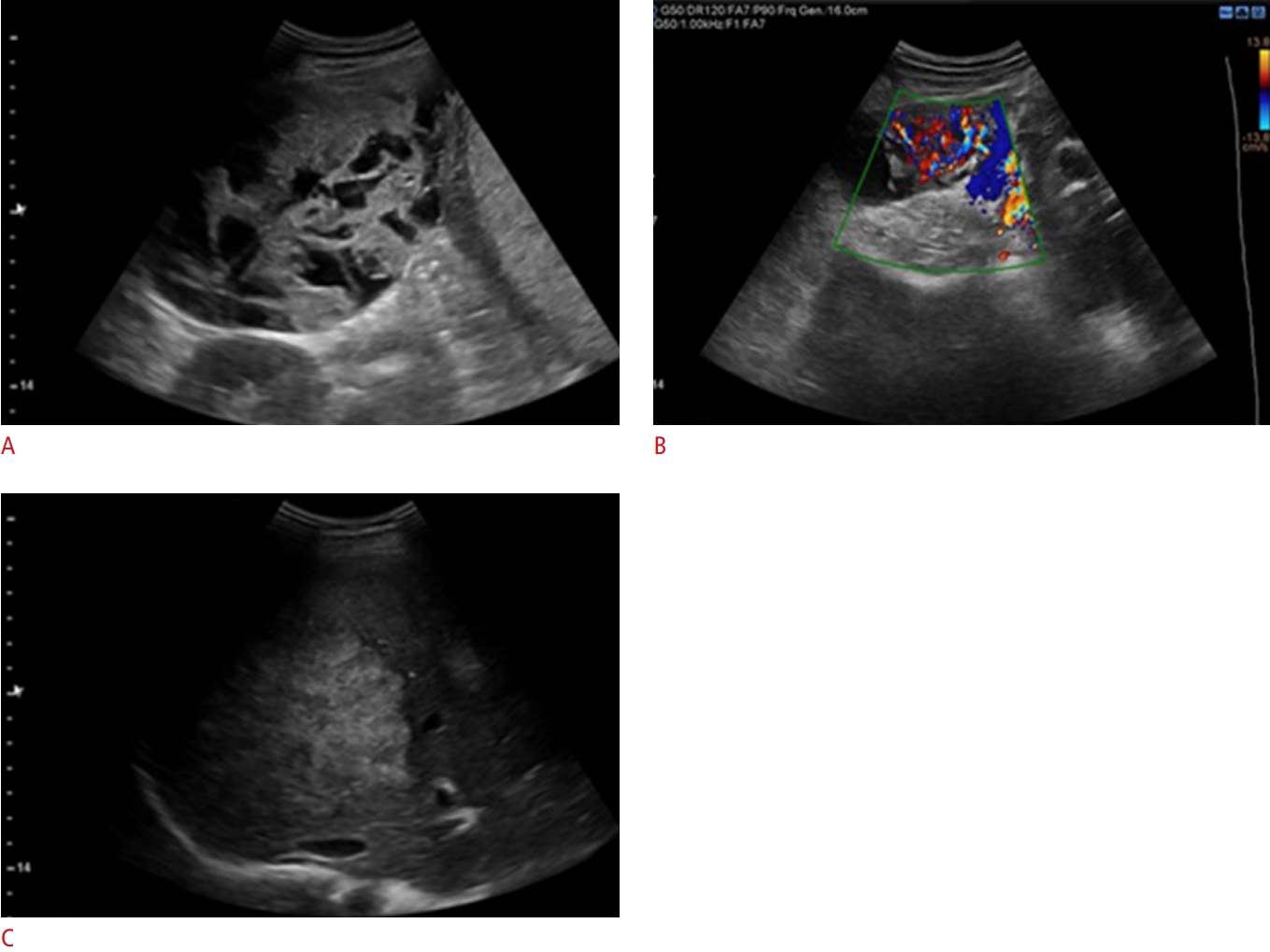 Fig.┬Ā4.Two non-simple unilocular lesions classified as O-RADS category 4.A. A unilocular lesion is noted in the left ovary of a 67-year-old woman with a solid component and without papillary projections. Color Doppler assessment has no role in the classification of unilocular lesions. The definite diagnosis of the lesion is a benign serous tumor. B. A paraovarian unilocular lesion is depicted in a 36-year-old woman with two papillary projections. A borderline epithelial tumor was reported as the final diagnosis. O-RADS, Ovarian-Adnexal Reporting and Data System.
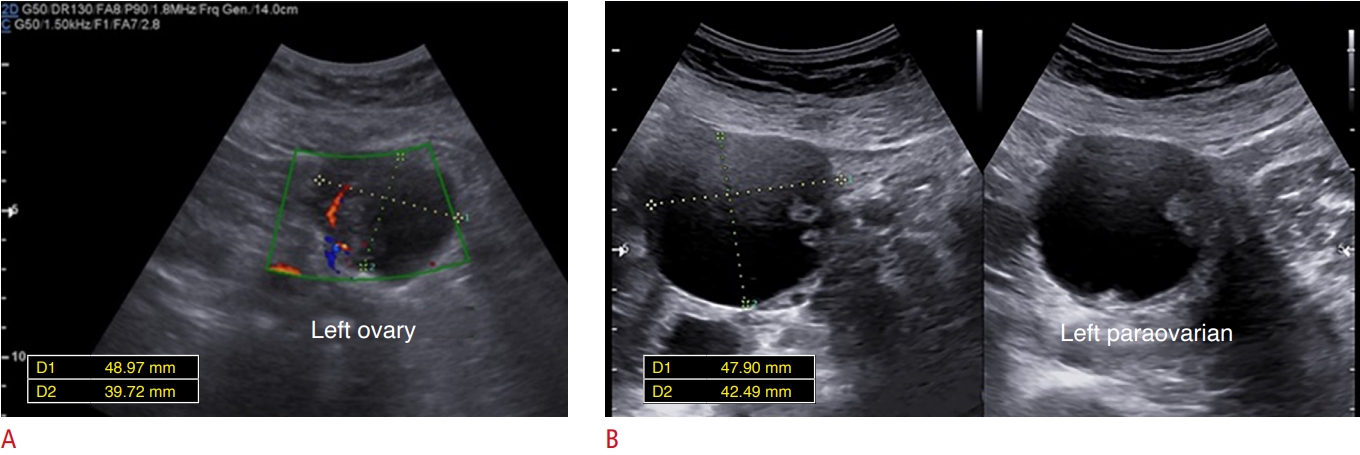 Fig.┬Ā5.A multilocular ovarian lesion with a solid component classified as O-RADS category 4 due to the absence of vascularity in color Doppler imaging.AŌĆōC. A 108├Ś66 mm multilocular ovarian lesion with a solid component measuring 21.5├Ś8.7 mm in a 30-year-old woman is depicted. B, C. The solid component has no vascularity in the color Doppler assessment. A color score of 1 in a multilocular ovarian lesion equals O-RADS category 4. O-RADS, Ovarian-Adnexal Reporting and Data System.
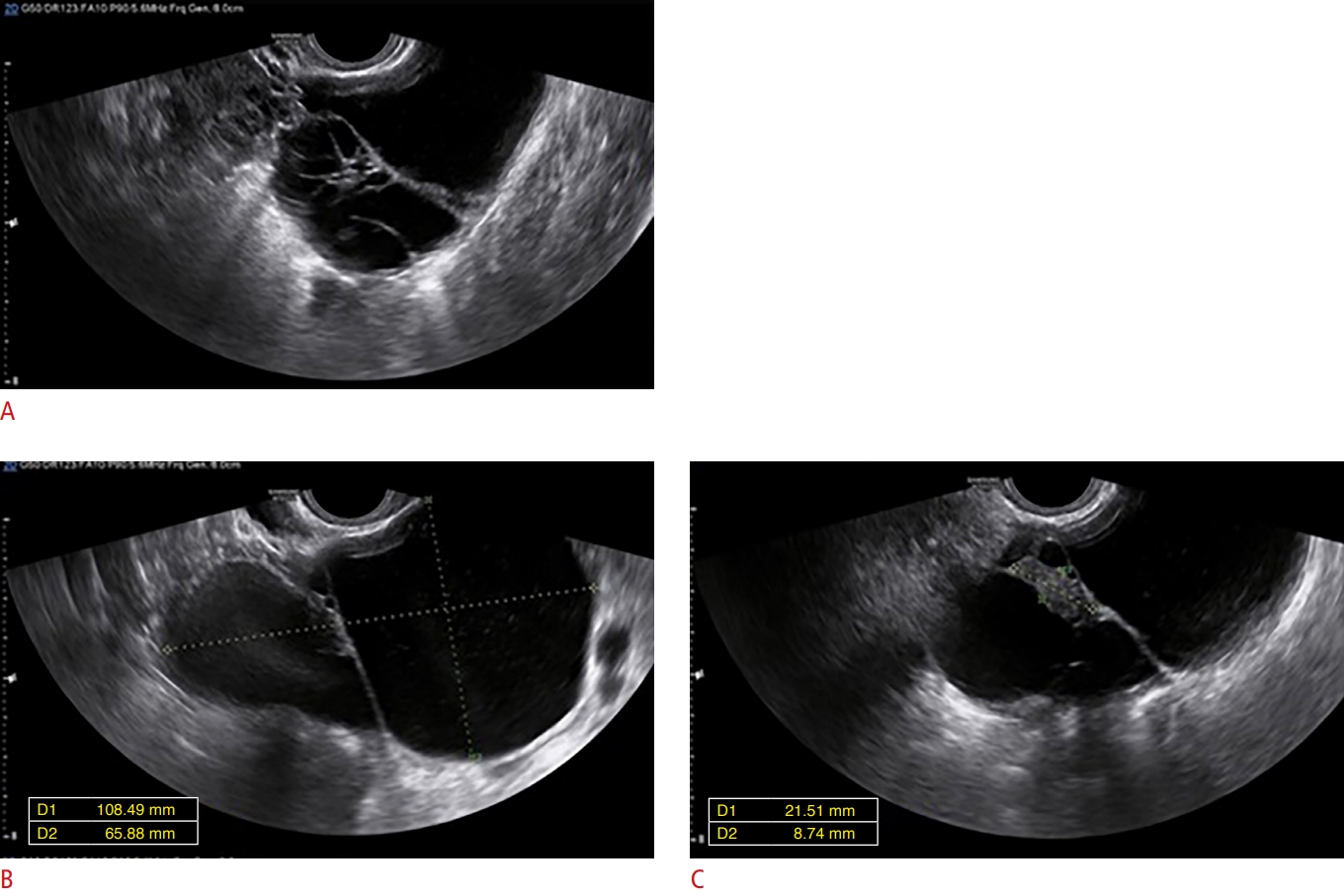 Fig.┬Ā6.A multilocular ovarian lesion with a smooth inner margin and without a solid component, classified as O-RADS category 3 due to the lack of vascular flow in color Doppler imaging.A. An ovarian lesion in a 41-year-old woman is depicted. B. It is classified as O-RADS category 3 based on its size and the lack of vascular flow in the color Doppler assessment. O-RADS, Ovarian-Adnexal Reporting and Data System.
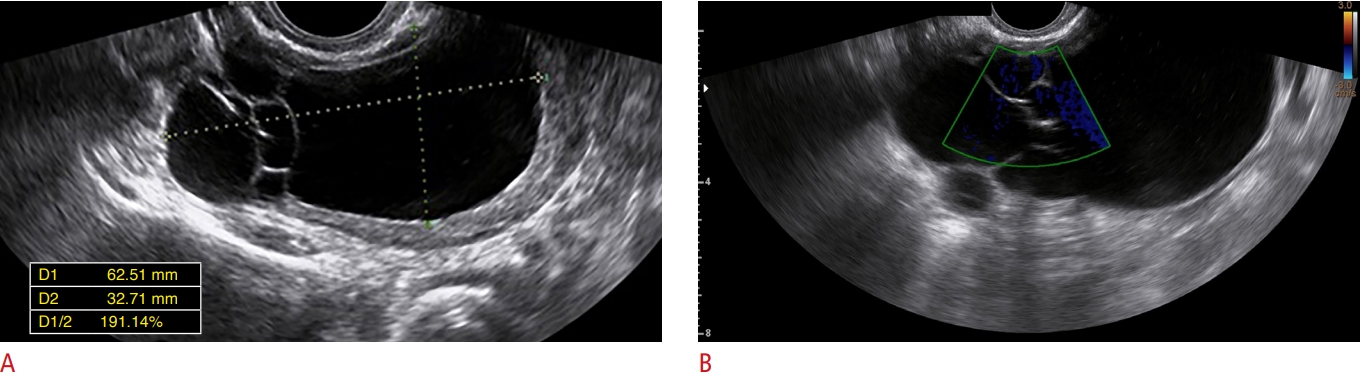 Fig.┬Ā7.A multilocular ovarian lesion with a solid component classified as O-RADS category 5 due to the presence of ascites and a peritoneal nodule.A. A multilocular ovarian lesion with a solid component is detected in a 40-year-old woman. B. The solid component has minimal flow in the color Doppler evaluation. C. The findings would individually support classifying the lesion as O-RADS category 4, but the presence of ascites and a peritoneal nodule (arrow) measuring 8.5 ├Ś 3 mm indicated a higher risk of malignancy, and the lesion was classified as O-RADS category 5. The pathological diagnosis was high-grade serous carcinoma. O-RADS, Ovarian-Adnexal Reporting and Data System.
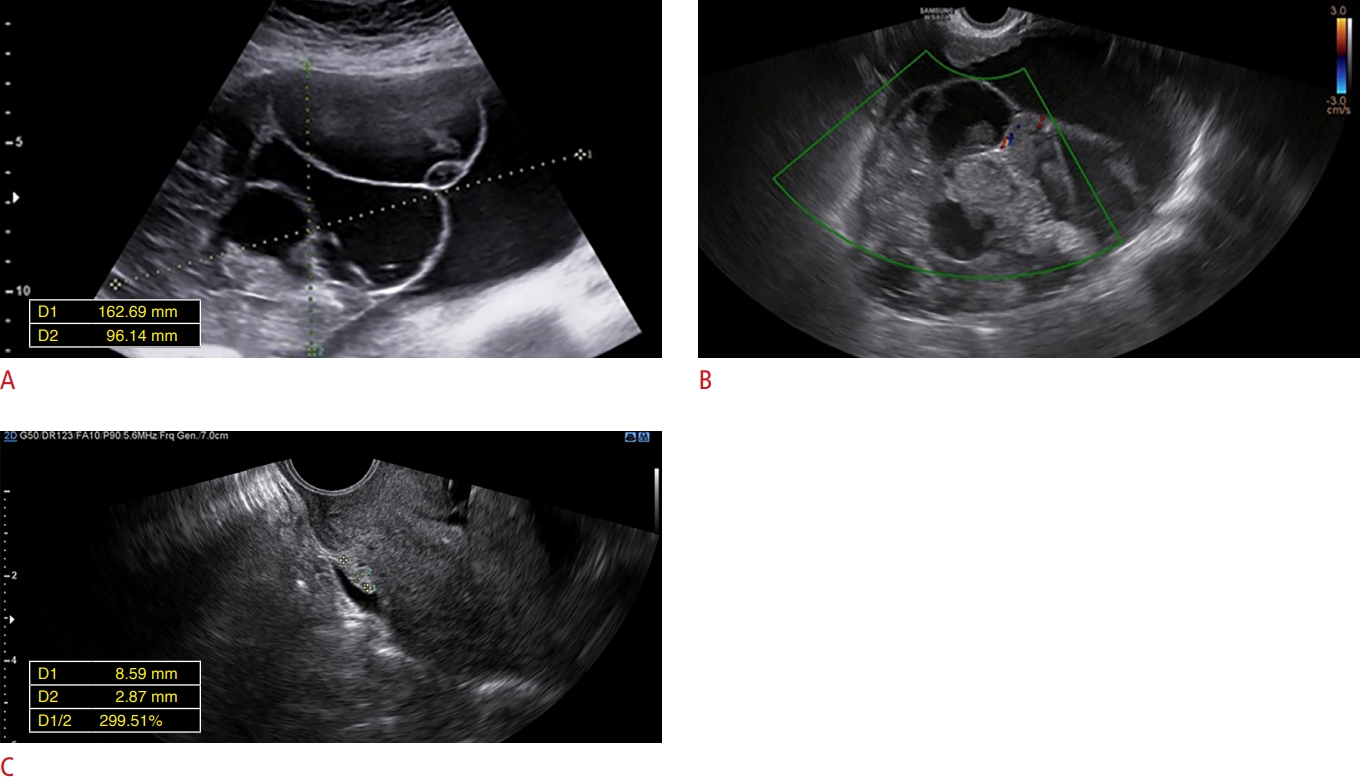 Fig.┬Ā8. |