AbstractPurposeAlthough the taller-than-wide (TTW) sign has been regarded as one of the most specific ultrasound (US) features of thyroid malignancy, uncertainty still exists regarding the US probe’s orientation when evaluating it. This study investigated which US plane would be optimal to identify the TTW sign based on malignancy risk stratification using a registry-based imaging dataset.
MethodsA previous study by 17 academic radiologists retrospectively analyzed the US images of 5,601 thyroid nodules (≥1 cm, 1,089 malignant and 4,512 benign) collected in the webbased registry of Thyroid Imaging Network of Korea through the collaboration of 26 centers. The present study assessed the diagnostic performance of the TTW sign itself and fine needle aspiration (FNA) indications via a comparison of four international guidelines, depending on the orientation of the US probe (criterion 1, transverse plane; criterion 2, either transverse or longitudinal plane).
ResultsOverall, the TTW sign was more frequent in malignant than in benign thyroid nodules (25.3% vs. 4.6%). However, the statistical differences between criteria 1 and 2 were negligible for sensitivity, specificity, and area under the curve (AUC) based on the size effect (all P<0.05, Cohen’s d=0.19, 0.10, and 0.07, respectively). Moreover, the sensitivity, specificity, and AUC of the four FNA guidelines were similar between criteria 1 and 2 (all P>0.05, respectively).
Ultrasonography (US) has been used as a first-line diagnostic tool to assess the malignancy risk of thyroid nodules [1-3]. Similar to other malignant US features, the taller-than-wide (TTW) sign, which occurs when the anteroposterior diameter of a thyroid nodule is greater than its transverse diameter (sometimes referred to as a non-parallel orientation) has been previously validated [4-11]. It has been used as one of the most specific US features indicating a high risk of thyroid malignancy in the current risk stratification systems (RSSs) [2,3,12-16].
However, a substantial debate has continued regarding the orientation of the US probe to determine the presence or absence of the TTW sign owing to its relatively low sensitivity (range, 14.6% to 68.0%) despite its high specificity (range, 82.1% to 100.0%) [4-8,11]. For example, the TTW sign is defined on the transverse plane in the American Association of Clinical Endocrinologists (AACE)/American College of Endocrinology (ACE)/Associazione Medici Endocrinologi (AME) system, the American Thyroid Association (ATA) system, and the American College of Radiology (ACR) Thyroid Imaging Reporting and Data System (TIRADS) [2,12,13]. Conversely, the TTW sign is defined on either the transverse or longitudinal plane by the Korean-TIRADS, European-TIRADS, and Chinese-TIRADS [3,14,15]. However, the British Thyroid Association system (BTA) does not clearly mention the plane [16].
In the 2021 modified Korean-TIRADS, the committee of the Korean Society of Thyroid Radiology selected the transverse plane as the only reference plane to define nodule orientation instead of the transverse or the longitudinal plane [17]. Recently, Kim et al. [6] reported that additional longitudinal US probe orientation did not significantly improve the diagnostic performance for the TTW sign compared to the conventional examination with the transverse plane to determine thyroid malignancy using five international RSSs; however, that study was primarily limited to the experience of two radiologists in a single institution. Until now, the effect of the reference US image plane has not been validated on the diagnostic performance of RSSs in a large, multicenter study. Therefore, this study analyzed data from a previous multicenter study in which 17 academic radiologists validated the diagnostic performance of the modified Korean-TIRADS using a registry-based imaging dataset [18,19].
This was a registry-based, multi-institutional, retrospective study. To establish an improved management guideline for patients with thyroid nodules and cancer, the Committee of the Korean Society of Thyroid Radiology has developed a web-based platform, known as the Thyroid Imaging Network of Korea registry, by gathering US images of thyroid nodules and their corresponding diagnoses from 26 different hospitals. With the efficient handling of imaging data and medical records, researchers can easily access a web-based program (AIM AiCRO, https://study.aim-aicro.com) that meets the strictest standards of data encryption and site-side security at the browser and server levels.
After receiving institutional review board approval, consecutive patients who had undergone thyroid US at the participating hospitals in the period between June 2015 and September 2015 were enrolled. The inclusion criteria were as follows: (1) nodules ≥1 cm in size, (2) the performance of fine needle aspiration (FNA), core-needle biopsy (CNB), or surgery for nodules, and (3) optimal US image quality for the evaluation of US features. All high-resolution images were captured at the maximum diameter of the thyroid nodule by the radiologists dedicated to thyroid imaging, who did not participate in the image analysis, using a US machine equipped with a 10-12 or 5-14 MHz linear probe. Representative paired US image files of each thyroid nodule were stored on the platform after deleting personally identifiable information from individual images.
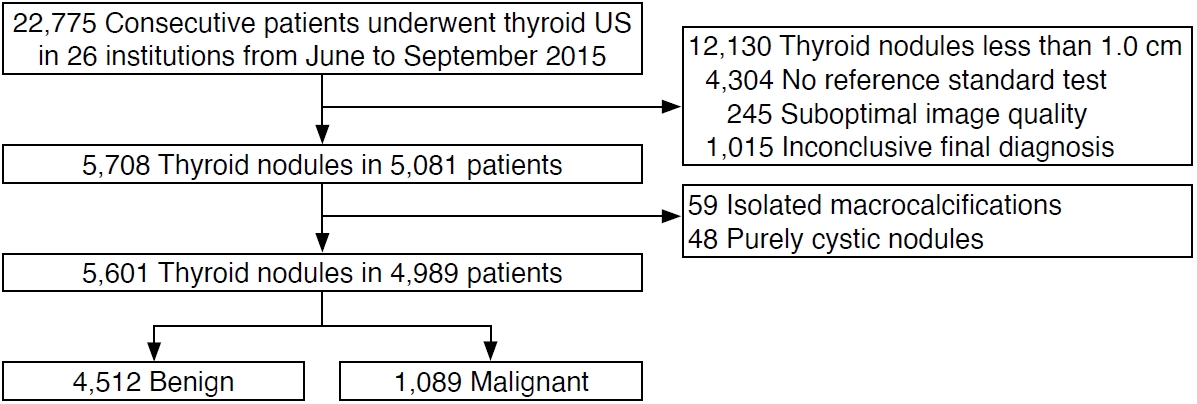
Among the 22,775 nodules, 16,679 were excluded because of the size of the thyroid nodules (<1.0 cm, n=12,130), the lack of a reference standard test (biopsy or surgery) (n=4,304), or suboptimal image quality (n=245). In addition, 1,102 nodules in 1,015 patients were excluded because of the inconclusive biopsy results. The US characteristics could not be analyzed in 59 isolated macrocalcifications (entirely calcified nodules) and 48 purely cystic nodules, so they were excluded. The remaining 4,989 consecutive patients with 5,601 thyroid nodules (≥1 cm) were included in this study (4,101 women, 888 men; median age, 54 years; age range, 19-76 years) (Fig. 1). The final diagnosis of nodules was determined by the surgical histologic diagnosis and definite CNB or FNA results.
Training sessions were conducted for the participating radiologists to establish a baseline consensus concerning the US features using the images of 15 biopsy-proven thyroid nodules that were not included in the study. Afterward, each of the 17 radiologists, having 8-22 years of experience in performing thyroid US, who had no knowledge of the final diagnosis for the corresponding thyroid nodules, conducted a separate retrospective image analysis. The radiologists were requested to fill in a multiple-answer electronic questionnaire for each set of images using the US lexicons as described in the four published guidelines [3,12-14].
Composition, echogenicity, shape, orientation, margin, calcification (echogenic foci), the intracystic comet-tail artifact, and spongiform appearance were assessed. To identify the TTW sign, all thyroid nodules were evaluated on both the transverse and longitudinal US planes. According to the US probe orientation, the presence of the TTW sign was defined as the anteroposterior diameter of a nodule being longer than its transverse diameter on the transverse plane or its longitudinal diameter on the longitudinal plane (Figs. 2-4). Two criteria were designated regarding the TTW sign on the transverse and longitudinal planes, as follows: (1) the presence of the TTW sign was determined only on the transverse plane; (2) the presence of the TTW sign was determined on either the transverse or longitudinal plane, similar to the recently published study by Kim et al. [6].
Of the four RSSs that were analyzed, the AACE/ACE/AME guidelines and ACR-TIRADS use criterion 1, while Korean Thyroid Imaging Reporting and Data System (K-TIRADS) and European Thyroid Imaging Reporting and Data System (EU-TIRADS) use criterion 2 [3,12-14]. For example, nodules with the TTW sign found on only the longitudinal plane would be categorized as negative by criterion 1, but positive by criterion 2. In the ACR-TIRADS, which uses a standardized scoring system to provide additional points for questionable US features of thyroid nodules, the TTW sign is awarded 3 points and the total score is determined by summing all the points from each category (composition, echogenicity, shape, margin, echogenic foci) [13]. Nodules having 3 points were classified as mildly suspicious, those with 4-6 points were classified as moderately suspicious, and those with ≥7 points were classified as highly suspicious [13].
In the K-TIRADS, the size threshold for biopsy is 1.5 cm for low-suspicion (K-TIRADS 3) nodules and 1.0 cm for intermediate-suspicion (K-TIRADS 4) or high-suspicion nodules (K-TIRADS 5) [3]. The biopsy size thresholds are 2.0 cm for intermediate-risk nodules (class 2) and 1.0 cm for high-risk nodules (class 3) in the AACE/ACE/AME guidelines [12]. The size threshold for biopsy in the ACR-TIRADS is 2.5 cm for mildly suspicious nodules (TR3), 1.5 cm for moderately suspicious nodules (TR4), and 1.0 cm for highly suspicious nodules (TR5) [13]. In the EU-TIRADS guidelines, the biopsy size threshold is 2.0 cm for low-risk nodules (EU-TIRADS 3), 1.5 cm for intermediate-risk nodules (EU-TIRADS 4), and 1.0 cm for high-risk nodules (EU-TIRADS 5) [14].
The diagnostic value of the TTW sign and FNA criteria of the four RSSs according to the TTW sign criteria was evaluated using the following metrics: sensitivity, specificity, positive predictive value, negative predictive value, and area under the receiver operating characteristic curve (AUC). Statistical analyses were performed using SPSS for Windows (version 24.0, IBM Corp., Armonk, NY, USA) and MedCalc version 19.1.3 (Ostend, Belgium). Statistical significance was set at P<0.05. Cohen’s d was used as one of the most common ways to calculate the effect size of the standardized difference between two mean values [20,21]. By convention, a Cohen’s d value of 0.2 represents a small effect, a Cohen’s d value of 0.5 corresponds to a medium effect, and a Cohen’s d value of 0.8 indicates a large effect [22].
The size of thyroid nodules ranged between 10 and 100 mm (interquartile range, 13.0 to 25.0 mm; median, 17.0 mm). Among the 5,601 selected nodules, 4,512 (80.6%) were benign, and 1,089 (19.4%) were malignant. Based on the final diagnosis determined by surgery or CNB (n=927) or FNA (n=162), the malignant nodules were classified into 989 papillary thyroid carcinomas (PTCs) (90.8%), and 100 other malignant tumors (9.2%). The other tumors included 62 follicular carcinomas (5.7%), 12 medullary thyroid carcinomas (1.1%), seven poorly differentiated carcinomas (0.6%), six anaplastic carcinomas (0.6%), five metastatic tumors (0.5%), four unspecified malignancies (0.4%), three lymphomas (0.3%), and one squamous cell carcinoma (0.1%). The final diagnosis of benign nodules was made through (1) the pathological results of surgical resection (n=390), (2) at least two benign diagnoses on FNA or CNB (n=594), and (3) one benign diagnosis on FNA or CNB (n=3,528). From the surgical reports of the 390 benign nodules, there were 239 cases of nodular hyperplasia, 135 follicular adenomas, eight cases of thyroiditis, one Hürthle cell adenoma, one intrathyroidal parathyroid, one simple cyst, one intrathyroidal thyroglossal duct cyst, one hemorrhagic degenerated lesion, one cellular adenomatoid nodule, one nodular hyperplasia or follicular adenoma, and one unspecified benign lesion.
Table 1 shows the prevalence of the TTW sign detected in thyroid nodules according to the US image planes. Of the 5,601 thyroid nodules, the TTW sign was found in only 0.4% of nodules on the longitudinal plane alone, 6.0% on the transverse plane alone, and 2.2% on both the transverse and longitudinal planes. The risk of malignancy was significantly higher in thyroid nodules with the TTW sign than in those without the TTW sign on the transverse plane alone, the longitudinal plane alone, and both the transverse and longitudinal planes (all P<0.001).
The diagnostic value of both TTW sign criteria for predicting thyroid malignancy is summarized in Table 2. Similar to previous studies with the TTW sign, the specificity was substantially high (95.5% for criterion 1, 95.4% for criterion 2), while the sensitivity was very low (24.0% for criterion 1, 25.3% for criterion 2), whether it was determined only on the transverse plane or either the transverse or longitudinal plane. Nonetheless, the accuracy was very high (81.6% for criterion 1, 81.7% for criterion 2). Compared to the method of determining the TTW sign only on the transverse US plane, the sensitivity, specificity, and AUC obtained when the TTW sign was judged on either the transverse or longitudinal plane presented statistically significant differences (P<0.001, P=0.016, and P=0.001, respectively); however, the observed differences were small considering the effect size based on Cohen’s d (d=0.19, d=0.10, and d=0.07, respectively).
Table 3 demonstrates the diagnostic performance of the FNA criteria according to the four guidelines as per the TTW sign criteria. The sensitivity, specificity, and AUCs of all four guidelines showed no significant differences (all P>0.05, respectively) according to the TTW sign criteria. The observed difference between criteria 1 and 2 in the sensitivity of FNA for malignancy in each RSS was minimal (0%-0.4%).
From the Korean registry-based imaging data, the diagnostic performance of the TTW sign for predicting thyroid malignancy was not different according to whether it was determined only on the transverse plane or additionally on the longitudinal plane. Moreover, the sensitivity, specificity, and AUC were nearly the same across the four international FNA criteria. These results support using the transverse plane for US determinations of the TTW sign of thyroid nodules.
Although a multicenter study revealed moderate interobserver agreement for the TTW sign (mean Cohen kappa=0.47) to diagnose PTC [23], its relatively low sensitivity (range, 14.6% to 68.0%) still remains problematic despite its high specificity (range, 82.1% to 100.0%) [4-8,11]. To improve the diagnostic performance of the TTW sign, two earlier studies clearly recommended using a combination of the transverse and longitudinal planes to determine the TTW sign of thyroid nodules during US examinations (Table 4) [5,11]. Moon et al. [5] reported in a study of 471 thyroid nodules that the AUC in which the TTW was determined either on the transverse or longitudinal plane was significantly higher than that only on the transverse or the longitudinal plane (P=0.006 and P=0.036, respectively). In addition, similar results were obtained with 942 thyroid nodules measuring 1 cm or smaller [11]. In that study, the TTW sign was detected on the transverse plane alone (n=100), the longitudinal plane alone (n=61), or both planes (n=131), and the accuracy of the TTW sign determined on either the transverse or the longitudinal plane was significantly higher than that on a single plane, such as the transverse or longitudinal plane alone, as well as both planes (0.544, 0.531, 0.627, and 0.702, respectively; P<0.05). However, Kim et al. recently reported that the diagnostic performance of four international RSSs was not significantly altered according to the US planes used to determine the TTW sign, based on the experience of two independent radiologists working at the same hospital [6]. They preferred the transverse orientation over the longitudinal orientation, which could induce more substantial interobserver variability related to different individuals’ neck contours and operators’ skills in tilting the US probes [6].
Therefore, it is crucial to decide in which direction the US probe is placed over the thyroid nodule to obtain two measurements, one parallel and the other perpendicular to the direction of wave propagation. This contrasts with other malignant US criteria including hypoechogenicity, microcalcifications, and irregular margins, which are completely unaffected by the direction of the probe. There is a lack of consensus in the current international guidelines on the reference US image plane to be used to determine the TTW sign. While some guidelines do not clearly mention the US plane to be used, other guidelines either recommend using the transverse plane alone or recommend either the transverse or the longitudinal plane [2,3,12-16].
This study further assessed the diagnostic performance of the TTW sign according to the US probe orientation using a sufficient number of cases (i.e., a Korean nationwide collected image set of 5,601 thyroid nodules with sizes ≥1 cm) that were previously assessed by 17 Korean thyroid-experienced radiologists. In the registry-based data, the prevalence of thyroid nodules with the TTW sign detected on the longitudinal plane alone was 0.4% (21/5,601), similar to the study by Kim et al. [6], which reported a proportion of 0.6% (11/1,905), while much lower than the study by Moon et al. [5], which reported a prevalence of 3.6% (17/471) from single-institutional data. Exceptionally, Moon et al. [5] considered the TTW sign to be present even if the anteroposterior and transverse diameters of thyroid nodules were the same. This is distinct from the definition of TTW as the anteroposterior diameter being longer than the transverse diameter [4,6-11], thus the exact number of thyroid nodules that satisfied the current definition of the TTW sign was still uncertain. Overall, adding a longitudinal examination led to a relatively negligible improvement in sensitivity (24.0% to 25.3% in the present study; 37.5% to 38.7% in the study by Kim et al. [6]; 58.4% to 68.0% in the study by Moon et al. [5]). As mentioned earlier, the diagnostic performance of the TTW sign for predicting thyroid malignancy was not significantly different in this study according to whether it was determined only on the transverse plane or additionally on the longitudinal plane. Moreover, the sensitivity, specificity, and AUC were nearly the same as per the four international FNA criteria. Accordingly, these results support a recent modification of the Korean-TIRADS guideline, according to which the transverse plane might be sufficient for evaluating the TTW sign, instead of the transverse or longitudinal plane as recommended in the previous version [1,3,17].
In 2002, Kim et al. [4] first introduced the concept of the TTW sign of thyroid nodules. It was defined as an anteroposterior diameter exceeding the transverse diameter. This has been considered a characteristic US feature that reflects the anti-gravitational growth pattern of thyroid malignancy across the normal tissue plane. Conversely, benign nodules usually grow along the tissue plane in a parallel fashion, similar to the patterns previously reported in breast US studies [24]. However, there are scarce data in the literature regarding the presence of a tissue plane in the thyroid gland. Several years later, Yoon et al. [25] reported that anteroposterior-transverse ratio (mean±standard deviation) of each thyroid nodule was significantly lower on transverse US images than on the corresponding computed tomography (CT) image (0.97±0.34 vs. 1.07±0.28, respectively; P<0.001); furthermore, the differences in the ratio between US and CT images were greater in benign nodules than in malignant nodules, owing to a shorter anteroposterior diameter on US. Since the shape and diameter displayed on US images may reflect the elasticity in response to an external force during probe compression, further reduction in thyroid nodules’ anteroposterior diameter may correspond to higher compressibility during US examinations. Generally, benign thyroid nodules tend to be more easily compressed than malignant nodules because of their lesser infiltration of the surrounding tissues [26-30]. In contrast, the various growth patterns of malignant cells including angiogenesis, destruction of thyroid follicles, reparative changes, fibrosis, and increased interstitial fluid pressure have been found to affect the US appearances of PTC by inducing greater stiffness compared to normal parenchyma or benign thyroid nodules, as has been validated in US elastography studies [26-31]. Consequently, dense fibrosis, which has been observed in 56%-89% of PTCs [32,33], has been suggested as the main mechanism of the TTW sign, which appears as no or less reduction of the anteroposterior diameter of malignant thyroid nodules on US images [25].
Based on those hypotheses, the diameter of malignant thyroid nodules parallel to the axis of transducer compression could appear longer than the diameter perpendicular to the axis of transducer compression in any direction the probe might point toward. However, considerable intra- and interobserver variability has been found in thyroid nodule measurements owing to differences in the transducer location, angulation, and pressure, as well as the manipulation of the calipers during the US image acquisition [6,34,35], which must be taken into account to determine the TTW sign. To confirm the accuracy of the TTW sign, more than 10 sonographers and some physicians recently recorded the diameters of 2,030 thyroid nodules in both the transverse and longitudinal orientations at six hospitals [36]. Measurements were performed under the rule that the transverse diameter in longitudinal and transverse sections was parallel to the skin, while the anteroposterior diameter was at a right angle to the transverse diameter. Despite a higher specificity and larger AUC of TTW on the longitudinal plane for diagnosing thyroid malignancy, data obtained from the transverse orientation were almost constant, whereas those from the longitudinal orientation frequently varied because the longitudinal axis changed slightly depending on the observer. Hence, their argument that the data obtained from transverse planes may be the most appropriate for multicenter collaborative research was consistent with this study, as well as an earlier study conducted by Kim et al. [6].
The current study has several limitations. First, 17 radiologists retrospectively determined the presence of the TTW sign from pairs of representative images uploaded from 26 different hospitals. These conditions are different from those of real clinical practice. Second, although specialized thyroid radiologists evaluated the US images of thyroid nodules after undertaking a training session to avoid misunderstanding the US lexicon, the interobserver agreement for the TTW sign was not assessed in this study. Third, because this study analyzed a previously filled-in multiple-answer electronic questionnaire by 17 radiologists, it was impossible to further analyze the influence of US probe tilting or neck contour during thyroid US examinations. To overcome these limitations, a multicenter validation study with a prospective design must be conducted.
In conclusion, a Korean registry-based study revealed that the longitudinal ultrasound probe orientation provided little additional diagnostic value for the TTW sign of thyroid nodules over the transverse orientation. Therefore, the transverse plane alone would be sufficient for evaluating the TTW sign to predict thyroid malignancy.
NotesAuthor Contributions Conceptualization: Lee YH, Kim JH, Na DG. Data acquisition: Kim JH, You SH, Shin JE, Kim SK. Data analysis or interpretation: Hong MJ, Lee YH, Na DG, Yang KS. Drafting of the manuscript: Hong MJ, Yang KS. Critical revision of the manuscript: Lee YH, Kim JH, Na DG, You SH, Shin JE, Kim SK. Approval of the final version of the manuscript: all authors. AcknowledgementsWe thank Dr. So Lyung Jung (Department of Radiology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea), Dr. Jung Hee Shin (Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine), Dr. Wooyul Paik (Department of Radiology, GangNeung Asan Hospital, University of Ulsan College of Medicine), Dr. Yeo Koon Kim (Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine), Dr. Chang Yoon Lee (Department of Radiology, Research Institute and Hospital, National Cancer Center), Dr. Eun Ju Ha (Department of Radiology, Ajou University School of Medicine), Dr. Younghee Yim (Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine), Dr. Nami Choi (Department of Radiology, Konkuk University Medical Center, Konkuk University School of Medicine), Dr. Hwa Seon Shin (Department of Radiology, Gyeongsang National University Hospital), Dr. Beomsu Kim (Department of Radiology, Kosin University Gaspel Hospital), Dr. Jin Yong Sung (Department of Radiology, Thyroid Center, Daerim St. Mary's Hospital), Dr. Hyun Jeong Kim (Department of Radiology, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea), Dr. Dae Bong Kim (Department of Radiology, Dongguk University Ilsan Hospital), Dr. Sun-Won Park (Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine; Department of Radiology, Seoul Metropolitan Government Seoul National University Boramae Medical Center), Dr. Ji Ye Lee (Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine), Dr. Hyun Kyung Lim (Department of Radiology, Soonchunhyang University Seoul Hospital), Dr. Ra Gyoung Yoon (Department of Radiology, Nowon Eulji Medical Center, Eulji University), Dr. Yoo Jin Lee (Department of Radiology, Busan Paik Hospital, Inje University College of Medicine), Dr. Joon Hyung Lee (Department of Radiology, Inje University Haeundae Paik Hospital), Dr. Hye Shin Ahn (Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine), Dr. Tae Yoon Kim (Department of Radiology, Hanyang University Guri Hospital, Hanyang University College of Medicine), Dr. Jee Young Kim (Department of Radiology, Eunpyeong St. Mary's Hospital), Dr. Jung Hwan Baek (Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine), Dr. Young Jun Choi (Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine), and Dr. Sae Rom Chung (Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine) for their participation in data collection.
References1. Lee JY, Baek JH, Ha EJ, Sung JY, Shin JH, Kim JH, et al. 2020 Imaging guidelines for thyroid nodules and differentiated thyroid cancer: Korean Society of Thyroid Radiology. Korean J Radiol 2021;22:840–860.
2. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1–133.
3. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol 2016;17:370–395.
4. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol 2002;178:687–691.
5. Moon HJ, Kwak JY, Kim EK, Kim MJ. A taller-than-wide shape in thyroid nodules in transverse and longitudinal ultrasonographic planes and the prediction of malignancy. Thyroid 2011;21:1249–1253.
6. Kim SY, Na DG, Paik W. Which ultrasound image plane is appropriate for evaluating the taller-than-wide sign in the risk stratification of thyroid nodules? Eur Radiol 2021;31:7605–7613.
7. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation: multicenter retrospective study. Radiology 2008;247:762–770.
8. Ren J, Liu B, Zhang LL, Li HY, Zhang F, Li S, et al. A taller-than-wide shape is a good predictor of papillary thyroid carcinoma in small solid nodules. J Ultrasound Med 2015;34:19–26.
9. Kim JY, Lee CH, Kim SY, Jeon WK, Kang JH, An SK, et al. Radiologic and pathologic findings of nonpalpable thyroid carcinomas detected by ultrasonography in a medical screening center. J Ultrasound Med 2008;27:215–223.
10. Kim JY, Kim SY, Yang KR. Ultrasonographic criteria for fine needle aspiration of nonpalpable thyroid nodules 1-2 cm in diameter. Eur J Radiol 2013;82:321–326.
11. Chen SP, Hu YP, Chen B. Taller-than-wide sign for predicting thyroid microcarcinoma: comparison and combination of two ultrasonographic planes. Ultrasound Med Biol 2014;40:2004–2011.
12. Gharib H, Papini E, Garber JR, Duick DS, Harrell RM, Hegedus L, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid modules--2016 update. Endocr Pract 2016;22:622–639.
13. Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol 2017;14:587–595.
14. Russ G, Bonnema SJ, Erdogan MF, Durante C, Ngu R, Leenhardt L. European Thyroid Association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur Thyroid J 2017;6:225–237.
15. Zhou J, Yin L, Wei X, Zhang S, Song Y, Luo B, et al. 2020 Chinese guidelines for ultrasound malignancy risk stratification of thyroid nodules: the C-TIRADS. Endocrine 2020;70:256–279.
16. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81 Suppl 1:1–122.
17. Heo YJ, Jeong HW, Kim D, Baek JW, Han JY, Choo HJ, et al. Usefulness of pointwise encoding time reduction with radial acquisition sequence in subtraction-based magnetic resonance angiography for follow-up of the Neuroform Atlas stentassisted coil embolization for cerebral aneurysms. Acta Radiol 2021;62:1193–1199.
18. Chung SR, Ahn HS, Choi YJ, Lee JY, Yoo RE, Lee YJ, et al. Diagnostic performance of the modified Korean Thyroid Imaging Reporting and Data System for thyroid malignancy: a multicenter validation study. Korean J Radiol 2021;22:1579–1586.
19. Ha EJ, Shin JH, Na DG, Jung SL, Lee YH, Paik W, et al. Comparison of the diagnostic performance of the modified Korean Thyroid Imaging Reporting and Data System for thyroid malignancy with three international guidelines. Ultrasonography 2021;40:594–601.
20. Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Individ Dif 2016;102:74–78.
21. Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ 2012;4:279–282.
23. Persichetti A, Di Stasio E, Coccaro C, Graziano F, Bianchini A, Di Donna V, et al. Inter- and intraobserver agreement in the assessment of thyroid nodule ultrasound features and classification systems: a blinded multicenter study. Thyroid 2020;30:237–242.
24. Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology 1995;196:123–134.
25. Yoon SJ, Yoon DY, Chang SK, Seo YL, Yun EJ, Choi CS, et al. "Tallerthan-wide sign" of thyroid malignancy: comparison between ultrasound and CT. AJR Am J Roentgenol 2010;194:W420–W424.
26. Monpeyssen H, Tramalloni J, Poiree S, Helenon O, Correas JM. Elastography of the thyroid. Diagn Interv Imaging 2013;94:535–544.
27. Kratky J, Vitkova H, Bartakova J, Telicka Z, Antosova M, Limanova Z, et al. Thyroid nodules: pathophysiological insight on oncogenesis and novel diagnostic techniques. Physiol Res 2014;63 Suppl 2:S263–S275.
28. Rago T, Scutari M, Loiacono V, Santini F, Tonacchera M, Torregrossa L, et al. Low elasticity of thyroid nodules on ultrasound elastography is correlated with malignancy, degree of fibrosis, and high expression of Galectin-3 and Fibronectin-1. Thyroid 2017;27:103–110.
29. Liu BJ, Li DD, Xu HX, Guo LH, Zhang YF, Xu JM, et al. Quantitative shear wave velocity measurement on acoustic radiation force impulse elastography for differential diagnosis between benign and malignant thyroid nodules: a meta-analysis. Ultrasound Med Biol 2015;41:3035–3043.
30. Chong Y, Shin JH, Ko ES, Han BK. Ultrasonographic elastography of thyroid nodules: is adding strain ratio to colour mapping better? Clin Radiol 2013;68:1241–1246.
31. Kim JH, Na DG, Lee H. Ultrasonographic echogenicity and histopathologic correlation of thyroid nodules in core needle biopsy specimens. Korean J Radiol 2018;19:673–681.
32. Isarangkul W. Dense fibrosis: another diagnostic criterion for papillary thyroid carcinoma. Arch Pathol Lab Med 1993;117:645–646.
33. Carcangiu ML, Zampi G, Pupi A, Castagnoli A, Rosai J. Papillary carcinoma of the thyroid: a clinicopathologic study of 241 cases treated at the University of Florence, Italy. Cancer 1985;55:805–828.
34. Lee HJ, Yoon DY, Seo YL, Kim JH, Baek S, Lim KJ, et al. Intraobserver and interobserver variability in ultrasound measurements of thyroid nodules. J Ultrasound Med 2018;37:173–178.
A 59-year-old woman with a papillary thyroid carcinoma showing the taller-than-wide sign on the transverse plane alone.Transverse ultrasonography shows a solid hypoechoic nodule with the taller-than-wide sign. B. Longitudinal ultrasonography shows the nodule parallel to the longitudinal axis of the thyroid gland.
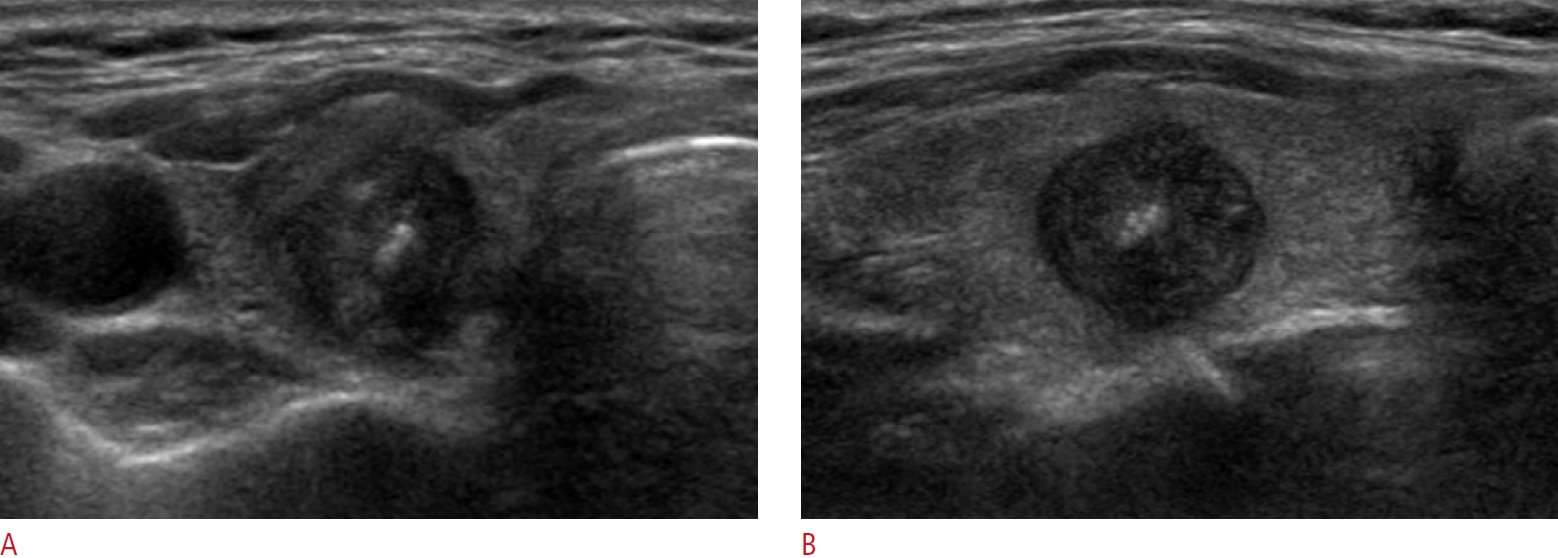 Fig. 2.A 53-year-old woman with papillary thyroid carcinoma showing the taller-than-wide sign on the longitudinal plane alone.Transverse ultrasonography shows a solid hypoechoic nodule parallel to the transverse axis of the thyroid gland. B. Longitudinal ultrasonography reveals the taller-than-wide orientation of the nodule.
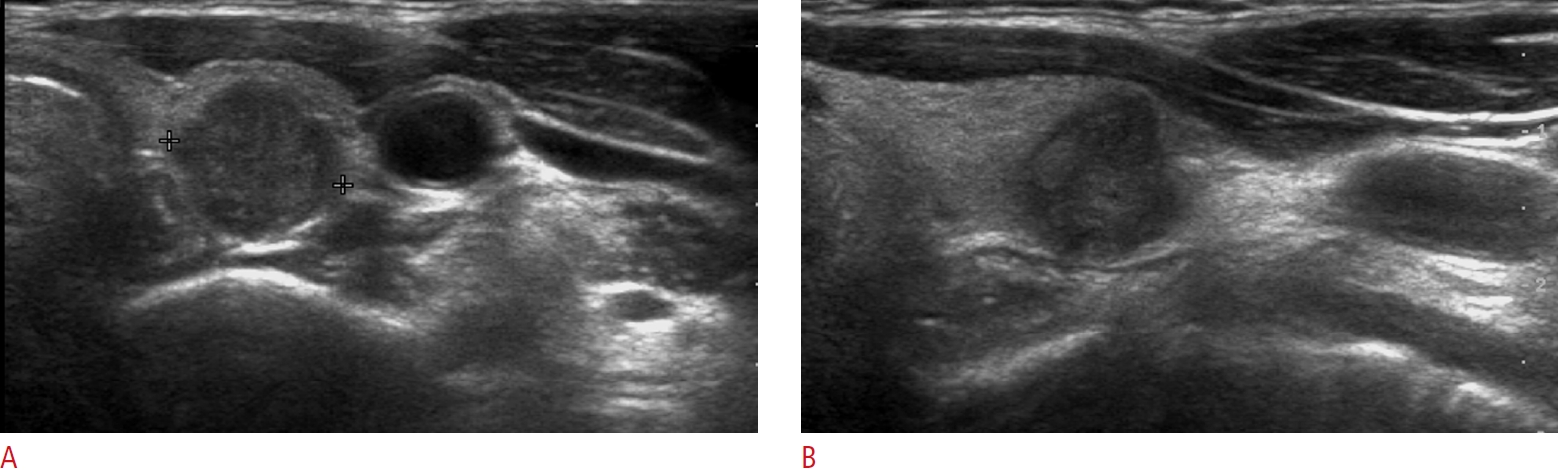 Fig. 3.A 41-year-old woman with papillary thyroid carcinoma with the taller-than-wide sign on both the transverse and longitudinal ultrasound planes.Transverse (A) and longitudinal (B) images show a solid hypoechoic nodule with the taller than-wide sign.
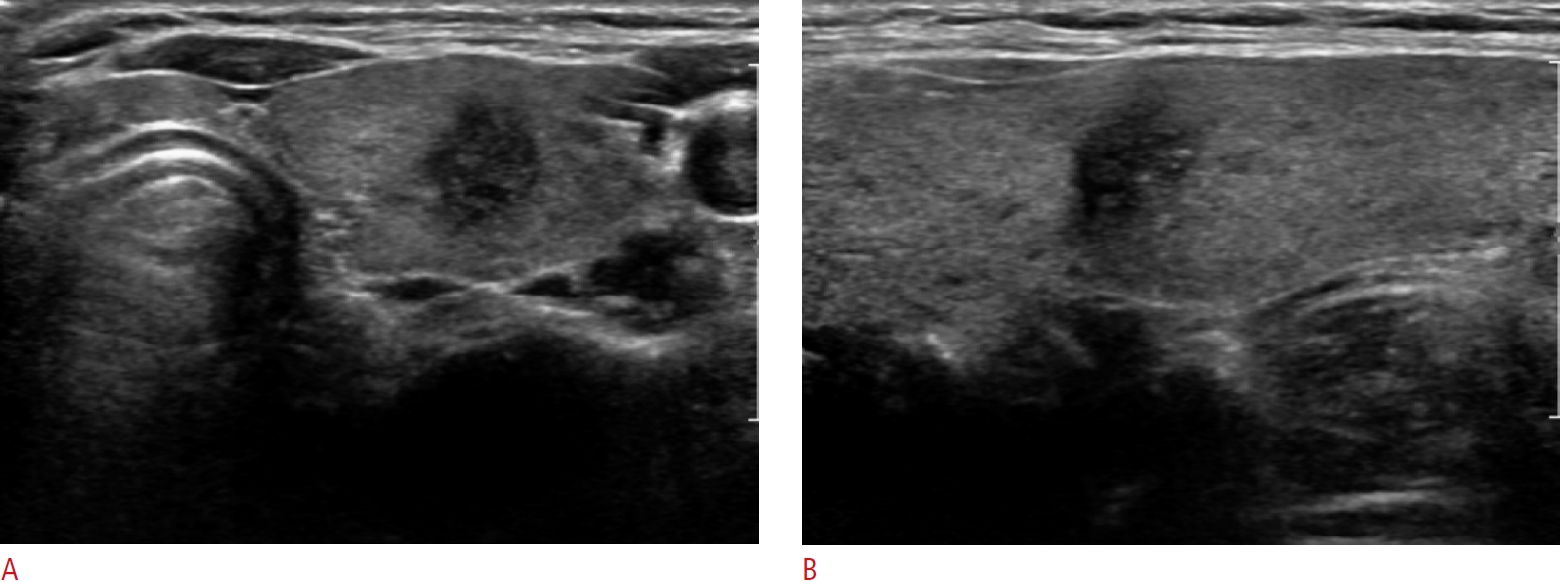 Fig. 4.Table 1.Prevalence of the taller-than-wide sign in thyroid nodules according to the US image plane Table 2.Diagnostic value of the taller-than-wide sign criteria for malignancy Table 3.Diagnostic performance of the FNA criteria of four guidelines according to taller-than-wide sign criteria Values in parentheses are presented as raw data unless otherwise indicated. Criterion 1: taller-than-wide sign on the transverse plane. Criterion 2: taller-than-wide sign on either the transverse or longitudinal plane. FNA, fine needle aspiration; AUC, area under the curve; CI, confidence interval; AACE/ACE/AME, American Association of Clinical Endocrinologists/American College of Endocrinology/Associazione Medici Endocrinologi; ACR-TIRADS, American College of Radiology Thyroid Imaging Reporting and Data System; EU-TIRADS, European Thyroid Imaging Reporting and Data System; K-TIRADS, Korean Thyroid Imaging Reporting and Data System. Table 4.Diagnostic performance of the taller-than-wide sign for predicting thyroid malignancy according to US criteria
Values in parentheses are presented as raw data unless otherwise indicated. Criterion 1: taller-than-wide sign on the transverse plane. Criterion 2: taller-than-wide sign on either the transverse or longitudinal plane. US, ultrasound; AUC, area under the curve; CI, confidence interval; M, malignant; B, benign; TTW, taller-than-wide; AP, anteroposterior; T, transverse. |
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||



 Print
Print facebook
facebook twitter
twitter Linkedin
Linkedin google+
google+
 Download Citation
Download Citation PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI




