AbstractPurposeHigh-contrast tissue characterization of thermal ablation has been desired to evaluate therapeutic outcomes accurately. This paper presents a photoacoustic (PA) characterization of thermal tissue ablation in the visible spectrum, in which higher light absorbance can produce spectral contrast starker than in the near-infrared range.
Methods
Ex vivo experiments were performed to measure visible PA spectra (480–700 nm) from fresh porcine liver tissues that received a thermal dose in a range of cumulative equivalent minutes at 43°C (CEM43). The local hemoglobin lobe area between 510–600 nm and whole-spectral area under the curve were evaluated to represent the transition of hemoglobin into methemoglobin (MetHb) in the target tissue.
ResultsThe thermal process below an estimated therapeutic CEM43 threshold (80–340 minutes) presented a progressive elevation of the PA spectrum and an eventual loss of local hemoglobin peaks in the visible spectrum, closer to the MetHb spectrum. Interestingly, an excessive CEM43 produced a substantial drop in the PA spectrum. In the spectral analysis, the visible spectrum yielded 13.9–34.1 times higher PA sensitivity and 1.42 times higher contrast change than at a near-infrared wavelength.
High-contrast characterization of thermal ablation has been desired to evaluate the therapeutic outcomes. The feasibility of high-contrast photoacoustic characterization of tissue ablation in the visible spectrum was demonstrated. The ex vivo study presents promising spectral features that can characterize and confirm thermal ablation.
Thermal therapeutic methods have long been effective options for cancer treatment over surgical treatment, with clear benefits of shorter hospitalization, lower cost, no need for general anesthesia, less bleeding and faster recovery, and a lower risk of postoperative complications [1]. There are several thermal therapeutic methods based on distinct modalities: radiofrequency ablation (RFA) using electric current, photothermal therapy (PTT) using light absorbance of biological tissue, and high-intensity focused ultrasound (HIFU) using mechanical interactions with the biological tissue. For these methods, an accurate therapeutic evaluation is crucial for safe ablation accurately spanning negative tumor margins to prevent undesired post-treatment tumor recurrence.
Medical technologies have made enormous advances in characterizing the properties of tissue that underwent thermal treatment; however, conventional methods face challenges. Magnetic resonance imaging (MRI) can provide high accuracy in evaluating thermal treatment [2]. However, it suffers from bulky, complex, and slow imaging sequences with limited device throughput, leading to high costs. Computed tomography can also visualize high-resolution morphology and real-time temperature changes in biological tissue [3]. However, it is still bulky, complex, and slow, mirroring the disadvantages of MRI as mentioned above, and more critically, its ionizing effect makes it an unfavorable option for repetitive sessions. Ultrasound (US) imaging can provide real-time guidance to accurately identify the position of the RFA tip or HIFU focus, but it does not provide a mechanism for exclusive contrast on tissue ablation.
Photoacoustic (PA) imaging is an emerging non-invasive modality that can combine rich optical contrast with acoustic submillimeter spatial resolution and centimeter-scale imaging depth [4]. An imaging session starts with light energy traveling through the biological tissue, which will be absorbed by the tissue, given its local absorption coefficient. Instantaneous excitation with pulsed light energy will result in non-radiative relaxation as a form of local heat, which will then trigger thermal volume expansion that creates mechanical pressure under stress and thermal confinement. The mechanical energy propagates through the biological tissue to reach an acoustic sensor array to reconstruct the initial pressure map through dynamic receive beamforming, corresponding to the distribution of light absorption in the field. Several scientific and clinical applications have been proposed using the PA imaging modality to visualize endogenous and exogenous contrast in biological tissue. Representative examples include, but are not limited to, the PA imaging of electrophysiology [5–8] and neurovascular physiology [9–11] for a comprehensive understanding of how the brain works, as well as PA imaging of early cancer indicators and aggressive-type tumors to enhance current clinical outcomes [12–15]. Several studies have also extracted distinct PA spectral features reflecting thermal therapeutic progress [16,17]. The prior state-of-the-art in biomedical PA tissue characterization after ablation was limited to imaging in the near-infrared range (NIR, 700–900 nm); the visible spectrum has remained unexplored.
This study presents the PA spectral changes in biological tissue over the visible spectrum (490–700 nm) due to different stages of thermal tissue ablation. It was hypothesized that hemoglobin content would be a valuable contrast to reflect therapeutic outcomes as a highly absorptive protein in the body; in particular, it is known that blood chromophores under high temperature experience a transition into a modified species, methemoglobin (MetHb) [18]. This study also investigated whether PA characterization in the visible spectrum could bring benefits over the NIR range. For example, a higher PA sensitivity is expected in the visible range, given 69.9 times higher absorbance at a local hemoglobin peak at 576 nm than that of a NIR isosbestic point at 797 nm (Fig. 1) [19–21]. Any change in tissue and hemoglobin denaturalization and the transition to MetHb should appear over the high contrast resolution.
Fig. 2A shows the thermal therapeutic setup, using HIFU as a representative modality to produce a local temperature increase in a controlled spatiotemporal domain. Fresh ex vivo porcine liver tissue was obtained from a local butcher shop and used to represent a common organ for thermal therapy, which would also require deep therapeutic/monitoring depth. A commercial 0.55-MHz HIFU transducer (H230, Sonic Concepts Inc., Bothell, WA, USA) was installed on an XYZ stage (SGSP26-100 and SHOT-204MS, Sigma Koki, Co., Ltd., Tokyo, Japan) to produce multiple lesions on the liver tissue, and entire mechanical transitioning procedures were automated using LabVIEW software (National Instruments Corp., Austin, TX, USA). A continuous sine wave with 560-mVpp input voltage was generated using a function generator (AFG3102, Tektronix, Beaverton, OR, USA) and further amplified by 55 dB using a radiofrequency amplifier (1040L, Electronics & Innovation, Rochester, NY, USA).
Different stages in thermal therapeutic processes were induced by a range of HIFU durations: 0, 5, 10, 15, and 20 seconds. Considering the focal width of 1.3 mm in the HIFU system and its conduction, each segment had an approximately 10×10-mm2 area to minimize the overlap of thermal fields. The focal depth at 10.21 mm was posed at the surface of the liver tissue with a 3D-printed fixture filled with degassed water to allow separate quantification of the ground-truth temperature. Each segment was indicated by empty Tygon tubes in the PA/US imaging field of view (Fig. 2B).
A data logger thermometer (DT-8891C, CEM, Shenzhen, China) and a K-type wire sensor were used to measure temperature changes upon HIFU application to the ex vivo porcine liver tissue. The sensor was located near the therapeutic focus on the ex vivo tissue. From the temperature trace, the thermal dose was estimated by the metric of cumulative equivalent minutes at 43°C (CEM43), which is given by
where N is the total number of data, Ti is a temperature value measured at the i-th sampling duration ti. RCEM is a calibration coefficient: 0.5 and 0.25 for Ti above and below 43°C, respectively. CEM43 has been used as a convenient method to convert a time-variant temperature trace into an equivalent thermal exposure in time duration at 43°C. Note that CEM43 is a metric that is solely determined by the tissue temperature, making the follow-up analysis adjustable to any thermal mechanisms. The therapeutic CEM43 threshold for enough exposure to induce tissue ablation (
After thermal therapeutic sessions with a specific CEM43, the HIFU transducer was carefully removed, and a PA/US imaging probe was installed on the ex vivo tissue with a room-temperature acoustic coupling gel and water tank. The transition was performed and completed at a 40-minute post-HIFU time point. Therefore, the PA characterization could be performed when tissue temperature had stabilized at room temperature. Therefore, this study did not include any PA intensity variations due to ambient temperature. An Nd:YAG pump laser (Surelite III-10, Continuum Lasers Inc., Milpitas, CA, USA) equipped with an optical parametric oscillator (OPO, Surelite OPO Plus, Amplitude Laser, Pessac, France) was used to produce laser pulses at 10 Hz. The harmonic separator produced 355 nm as a pumping source, and OPO produced a wide range of visible-to-NIR wavelengths. The spectrum of interest was 490–700 nm at 10-nm intervals, and each energy was equalized using an energy sensor and meter (QE25LP-H-MB-D0 and Maestro, Gentec-EO Inc., Quebec, Canada). The laser pulses were delivered to a target subject by a customized, bifurcated optical fiber bundle (Fiberoptic Systems Inc., Simi Valley, CA, USA) designed for uniform light illumination in the lateral direction of the PA imaging probe. Acoustic data were obtained using a 5-MHz clinical linear array transducer (L7-4, Verasonics, Kirkland, WA, USA) between the bifurcated bar-type outlets of the optical fiber bundles, and the data were delivered to a US research package for recording (Vantage256, Verasonics). At each therapeutic segment, a tissue surface about 0.1-mm in thickness was identified based on the PA/US images, and a projected PA spectrum was derived. The design reflects the proposed scheme to deliver optical energy at a local therapeutic focus through intracorporeal light illumination for PA signal generation. At each CEM43, the PA spectra from three liver slices were collected.
To validate the thermal ablation in a range of CEM43 values, the cross-section of the therapeutic lesion was cut, and the surface layer was obtained for a histopathological analysis. A single liver was used to minimize variability in tissue properties. The samples were processed with hematoxylin and eosin (H&E) staining, and ×200 and ×400 microscopic images were analyzed to identify cellular-level clues of thermal tissue damage.
Our thermal therapeutic process was first characterized by temperature tracing at the therapeutic focus on the fresh ex vivo liver tissue surface. The trace was converted into the CEM43 metric, following Eq. (1). Fig. 3A shows the temperature increase in ex vivo liver tissue with continuous HIFU for 20 seconds. We estimated the total heat exposure of the ex vivo liver for each HIFU duration as follows (Fig. 3B): CEM43 values of 0, 0.2, 30.9, 637.2, and 3,466.3 minutes for HIFU durations of 0, 5, 10, 15, and 20 seconds, respectively. Considering the
Fig. 4A shows the calibrated PA spectra in the thermal therapeutic processes over the 490–700 nm range. In the control data (i.e., CEM43=0 minute), a clear hemoglobin spectrum was observed, with the local hemoglobin lobe centered at 560 nm (Fig. 1), indicating that oxygenated hemoglobin (HbO2) and deoxygenated hemoglobin (HbR) were the predominant absorbers in the fresh ex vivo liver tissue. As the thermal dose increased, the local hemoglobin peaks gradually lowered and became almost indistinguishable when CEM43 was longer than the
Based on previous studies [18,26], thermal ablation triggers a transition of blood chromophores into a modified species known as MetHb. The absorption spectrum of MetHb is known to present a higher absorbance in the visible range and complete loss of the hemoglobin peaks at 560 nm (Fig. 1) [20]. Due to these spectral features, it is suggested that the transition into MetHb could be quantitatively evaluated in terms of the “local hemoglobin lobe area,” which integrates the area of the PA spectrum between 510 nm and 600 nm (normalized at 510 nm) subtracted by the baseline area estimated by a straight line between the PA intensities at the wavelength range, as expressed by:
where SPA is the target PA spectrum of HbO2, HbR, or MetHb, B is the baseline under the straight line between the PA intensities between a target spectral range from λ1 to λN, which was from 510 nm to 600 nm in this study. Therefore, SPA (λ1) and SPA (λN) are equal to B (λ1) and B (λN). N is the number of wavelengths and is 10 with 10-nm intervals between 510 nm and 600 nm.
This range includes a local hemoglobin lobe centered at 560 nm; therefore, a positive area value is expected when HbO2 and/or HbR is dominant before the thermal treatment. However, MetHb does not have a lobe in the spectral range, so its predominance will remove the lobe within the spectral range. As a reference, the HbO2 and HbR spectra obtained from [19] and the MetHb spectrum obtained from Zijlstra et al. [27] produce local hemoglobin lobe areas at 10.4, 6.7, and −0.5, respectively (Fig. 5A). Only MetHb produces a negative area value close to zero in the spectral range, which can serve as a distinct feature in identifying the therapeutic progress. Fig. 5B shows the local hemoglobin lobe area value at each CEM43. In general, the local hemoglobin lobe area progressively decreased and formed an intercept into a negative value within the
Interestingly, there was a sudden global drop in the PA spectrum at the extreme CEM43 of 3,466.3 minutes (Fig. 4B). Moreover, the local hemoglobin lobe area value converged near zero, as shown in Fig. 5B, which means that there was no substantial presence of hemoglobin contents in the therapeutic focus. Based on these two observations, it is hypothesized that complete lysis or clearance of the hemoglobin contents at the therapeutic focus induced the sudden and dramatic change. Therefore, these results indicate a loss of the local hemoglobin lobe and intensity drop as potential metrics to evaluate the progressive thermal therapeutic process from mild to complete thermal ablation.
In a closer view, an optimal wavelength was determined to secure the maximal contrast resolution. The PA intensity at 490 nm was significantly higher than that at the NIR wavelength of 700 nm. The intensity ratio between 490 nm and 700 nm indicated 18.6, 16.4, 34.1, 21.3, and 13.9 times higher amplifications when CEM43 values were 0, 0.2, 30.9, 637.2, and 3,466.3 minutes, respectively. The PA signal at a wavelength longer than 490 nm did not improve contrast. Therefore, selecting a wavelength as short as possible in the visible spectral range (490–700 nm) would be a practical approach for securing a higher signal-to-noise ratio. The data also made it possible to evaluate the optimal wavelength range to identify the contrast change of the visible PA spectrum when CEM43 transitioned from below to above
Fig. 6A shows the H&E histopathologic images of the ablated liver tissue for different thermal exposure times. No thermal ablation was found with the CEM43 values under the
This paper presents the feasibility of the high-contrast PA tissue characterization of thermal ablation in the visible spectrum. An ex vivo evaluation using fresh porcine liver tissues showed a noticeable change in the visible PA spectrum when the CEM43 exceeded the
The efficacy of this technology is not limited to certain thermal therapeutic modalities (e.g., RFA, HIFU, PTT), but a careful design would be needed to maximize its clinical efficacy. For example, RFA already introduces a minimally invasive needle into the tumor and extends the electrodes for thermal generation throughout the volume, and US imaging guidance is involved in placing them in the proper position. In this case, implementing optical fibers to deliver the visible spectrum as one or few of the RFA electrodes could produce continuous monitoring of the volumetric RFA process without substantial changes in the clinical protocol, which has never been provided. Encouragingly, several predicate PA sensing devices have integrated either acoustic or optical sources in a needle or catheter. However, using an acoustic part near the heat source would be ineffective since it would be vulnerable to ambient heat deposition [28]. Conventional piezoelectric transducers only tolerate up to approximately 50°C [29], indicating that they are incapable of enduring high temperatures during thermal therapy. Special customizations for thermal isolation would be only achieved with substantial costs of large tool size, higher fabrication costs, and deterioration of acoustic properties [30]. In contrast, optical modality fibers can have higher heat tolerance, up to a few thousand degrees Celsius, based on readily available materials and coating techniques [31]. Other studies have tested configurations to isolate the light and acoustic components, but their clinical applications focused on tool tracking rather than providing a molecular tissue characterization feature to monitor dynamic interventional and/or therapeutic processes [32,33].
Many aspects still must be addressed to secure the translational practicality of this technique. The scope of this study did not yet cover real-time monitoring of thermal ablation during treatment—instead, ex vivo targets were controlled to sorely evaluate the visible PA spectral changes without the thermal effect, which would produce a significant intensity bias during the treatment process. The authors’ upcoming work will focus on advancing this technology toward a tool for real-time monitoring of the thermal ablation process. The authors plan to make a more comprehensive model that merges the PA thermometric and spectrometric capabilities to interpret the visible PA spectral changes as a function of local temperature. In the course of development, statistical rigor will be ensured by testing a vast number of ex vivo tissue samples for PA tissue characterization and H&E histopathology at a finer CEM43 resolution for tissue ablation. Immunohistochemistry will also be performed to validate the transition of hemoglobin into MetHb or further into complete lysis. For example, an excessive thermal dose is known to eventually denature MetHb [34], which might be the reason behind the rebound of the local hemoglobin lobe area with an excessive thermal dose (Fig. 5B).
There are differences between ex vivo and in vivo circumstances. In living tissue, blood flow may act like a coolant, which counteracts the thermal mechanism, leading to slower temperature increases during heating and faster cooling in the post-treatment period [21]. However, the efficacy of PA monitoring will be preserved because the contrast primarily depends on the tissue ablation status; nonetheless, a more thorough in vivo study using a preclinical model should be performed for complete validation. It is also planned to test for any potential interference due to other physiological changes resulting from thermal treatment, including immune and circulatory system responses [35,36].
Spectroscopic PA sensing could also be used for better localization of thermal therapy using an exogenous contrast agent targeting aggressive tumors. For instance, prostate-specific membrane antigen is a type-II integral cell-surface membrane protein that is overexpressed more in aggressive prostate cancer epithelium cells and the neovasculature of non-prostatic cancers (lung, kidney, colon, stomach, breast, and brain). Several promising studies have presented successful development and deployment of targeted contrast [37–39]. Integration of our PA treatment monitoring workflow with the contrast agent technology will lead to a novel framework that allows pre-treatment tissue characterization in the spatiospectral domain, leading to better thermal localization of target lesions.
AcknowledgmentsThis work was supported by (1) the Congressionally Directed Medical Research Programs, Department of Defense (DOD), USA (W81XWH-18-1-0188); (2) the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (1711137879, KMDF_PR_20200901_0009); (3) the Institute of Information & communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) (2022-0-00101).
NotesAuthor Contributions Conceptualization: Song TK, Kang J. Data acquisition: Song H. Data analysis or interpretation: Song H, Kang J. Drafting of the manuscript: Song H, Kang J. Critical revision of the manuscript: Song TK, Kang J. Approval of the final version of the manuscript: all authors. References1. Dai Q, Cao B, Zhao S, Zhang A. Synergetic thermal therapy for cancer: state-of-the-art and the future. Bioengineering (Basel) 2022;9:474.
3. Bruners P, Levit E, Penzkofer T, Isfort P, Ocklenburg C, Schmidt B, et al. Multi-slice computed tomography: a tool for non-invasive temperature measurement? Int J Hyperthermia 2010;26:359–365.
4. Wang LV, Hu S. Photoacoustic tomography: in vivo imaging from organelles to organs. Science 2012;335:1458–1462.
5. Rasheed NS, Cressman JR, Chitnis PV. Photoacoustic imaging of biopotentials: a feasibility study. Biomedical Optics 2016, Cancer Imaging and Therapy. 2016 Apr 25–28 Fort Lauderdale, FL, USA. Washington, DC: Optica Publishing Group, 2016:JW3A.56.
6. Rao B, Zhang R, Li L, Shao JY, Wang LV. Photoacoustic imaging of voltage responses beyond the optical diffusion limit. Sci Rep 2017;7:2560.
7. Kang J, Kadam SD, Elmore JS, Sullivan BJ, Valentine H, Malla AP, et al. Transcranial photoacoustic imaging of NMDA-evoked focal circuit dynamics in the rat hippocampus. J Neural Eng 2020;17:025001.
8. Kang J, Zhang HK, Kadam SD, Fedorko J, Valentine H, Malla AP, et al. Transcranial recording of electrophysiological neural activity in the rodent brain in vivo using functional photoacoustic imaging of near-infrared voltage-sensitive dye. Front Neurosci 2019;13:579.
9. Lv J, Li S, Zhang J, Duan F, Wu Z, Chen R, et al. In vivo photoacoustic imaging dynamically monitors the structural and functional changes of ischemic stroke at a very early stage. Theranostics 2020;10:816–828.
10. Kang J, Liu X, Cao S, Zeiler SR, Graham EM, Boctor EM, et al. Transcranial photoacoustic characterization of neurovascular physiology during early-stage photothrombotic stroke in neonatal pigletsin vivo. J Neural Eng 2022;18:065001.
11. Kang J, Boctor EM, Adams S, Kulikowicz E, Zhang HK, Koehler RC, et al. Validation of noninvasive photoacoustic measurements of sagittal sinus oxyhemoglobin saturation in hypoxic neonatal piglets. J Appl Physiol (1985) 2018;125:983–989.
12. Kang J, Kim EK, Kim GR, Yoon C, Song TK, Chang JH. Photoacoustic imaging of breast microcalcifications: a validation study with 3-dimensional ex vivo data and spectrophotometric measurement. J Biophotonics 2015;8:71–80.
13. Kang J, Chang JH, Kim SM, Lee HJ, Kim H, Wilson BC, et al. Real-time sentinel lymph node biopsy guidance using combined ultrasound, photoacoustic, fluorescence imaging: in vivo proof-of-principle and validation with nodal obstruction. Sci Rep 2017;7:45008.
14. Valluru KS, Wilson KE, Willmann JK. Photoacoustic imaging in oncology: translational preclinical and early clinical experience. Radiology 2016;280:332–349.
15. Luke GP, Yeager D, Emelianov SY. Biomedical applications of photoacoustic imaging with exogenous contrast agents. Ann Biomed Eng 2012;40:422–437.
16. Gao S, Ashikaga H, Suzuki M, Mansi T, Kim Y, Ghesu F, et al. Cardiacgated spectroscopic photoacoustic imaging for ablation-induced necrotic lesion visualization: in vivo demonstration in a beating heart Preprint at https://doi.org/10.1101/2022.05.23.492682
. 2022.
17. Gao S, Ashikaga H, Mansi T, Halperin HR, Zhang HK. Photoacoustic necrotic region mapping for radiofrequency ablation guidance. 2021 IEEE International Ultrasonics Symposium (IUS); 2021 Sep 11–16; Xi’an, China. New York: Institute of Electrical and Electronics Engineers, 2021. 21434991.
18. Lanka P, Francis KJ, Kruit H, Farina A, Cubeddu R, Sekar SK, et al. Optical signatures of radiofrequency ablation in biological tissues. Sci Rep 2021;11:6579.
19. Prahl S. Optical absorption of hemoglobin [Internet]. Scott Prahl 1999. [cited 2022 Oct 10]. Available from: omlc.org/spectra/hemoglobin
.
20. Zijlstra WG, Buursma A, Meeuwsen-van der Roest WP. Absorption spectra of human fetal and adult oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin, and methemoglobin. Clin Chem 1991;37:1633–1638.
21. Van Gastel M, Stuijk S, De Haan G. Camera-based pulse-oximetry: validated risks and opportunities from theoretical analysis. Biomed Opt Express 2018;9:102–119.
22. van Rhoon GC, Samaras T, Yarmolenko PS, Dewhirst MW, Neufeld E, Kuster N. CEM43 degrees C thermal dose thresholds: a potential guide for magnetic resonance radiofrequency exposure levels? Eur Radiol 2013;23:2215–2227.
23. Graham SJ, Chen L, Leitch M, Peters RD, Bronskill MJ, Foster FS, et al. Quantifying tissue damage due to focused ultrasound heating observed by MRI. Magn Reson Med 1999;41:321–328.
24. Quesson B, Laurent C, Maclair G, de Senneville BD, Mougenot C, Ries M, et al. Real-time volumetric MRI thermometry of focused ultrasound ablation in vivo: a feasibility study in pig liver and kidney. NMR Biomed 2011;24:145–153.
25. Chang IA. Considerations for thermal injury analysis for RF ablation devices. Open Biomed Eng J 2010;4:3–12.
26. Aizawa K, Sato S, Saitoh D, Ashida H, Obara M. In vivo photoacoustic spectroscopic imaging of hemoglobin derivatives in thermally damaged tissue. Jpn J Appl Phys 2009;48:062302.
27. Zijlstra WG, Buursma A, Falke HE, Catsburg JF. Spectrophotometry of hemoglobin: absorption spectra of rat oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin, and methemoglobin. Comp Biochem Physiology Part B Comp Biochem 1994;107:161–166.
28. Yang JM, Li C, Chen R, Zhou Q, Shung KK, Wang LV. Catheter-based photoacoustic endoscope. J Biomed Opt 2014;19:066001.
29. McNab A, Kirk KJ, Cochran A. Ultrasonic transducers for high temperature applications. IEEE Proc Sci Meas Technol 1998;145:229–236.
30. Kazys R, Vaskeliene V. High temperature ultrasonic transducers: a review. Sensors (Basel) 2021;21:3200.
31. Ma S, Xu Y, Pang Y, Zhao X, Li Y, Qin Z, et al. Optical fiber sensors for high-temperature monitoring: a review. Sensors (Basel) 2022;22:5722.
32. Piras D, Grijsen C, Schutte P, Steenbergen W, Manohar S. Photoacoustic needle: minimally invasive guidance to biopsy. J Biomed Opt 2013;18:070502.
33. Cheng A, Kim Y, Itsarachaiyot Y, Zhang HK, Weiss CR, Taylor RH, et al. Photoacoustic-based catheter tracking: simulation, phantom, and in vivo studies. J Med Imaging (Bellingham) 2018;5:021223.
34. Seto Y, Kataoka M, Tsuge K. Stability of blood carbon monoxide and hemoglobins during heating. Forensic Sci Int 2001;121:144–150.
35. Hu Z, Yang XY, Liu Y, Morse MA, Lyerly HK, Clay TM, et al. Release of endogenous danger signals from HIFU-treated tumor cells and their stimulatory effects on APCs. Biochem Biophys Res Commun 2005;335:124–131.
36. Faizullina DR, Grizunov VV, Berkovich AE. Blood flow modification attached to HIFU exposure mast cell degranulation. Reg Hemodyn Microcirc 2019;18:81–88.
37. Zhang HK, Chen Y, Kang J, Lisok A, Minn I, Pomper MG, et al. Prostate-specific membrane antigen-targeted photoacoustic imaging of prostate cancer in vivo. J Biophotonics 2018;11:e201800021.
Molar extinction spectra of oxygenated/deoxygenated hemoglobin (HbO2 and HbR) and methemoglobin (MetHb).
Data tips indicate arbitrary absorption coefficients at isosbestic points in the visible and near-infrared ranges (584 nm and 796 nm, respectively). Hemoglobin spectra were obtained from Prahl [19]. The MetHb spectrum was obtained from Zijlstra et al. [20], where coefficients were available at limited wavelengths: 450, 480, 500, 510, 520, 530, 540, 550, 560, 570, 580, 590, 600, 630, 660, 680, and 700 nm. The MetHb spectrum was scaled to have an intercept between HbR and MetHb at 660 nm based on their molar extinction spectra in Van Gastel et al. [21].
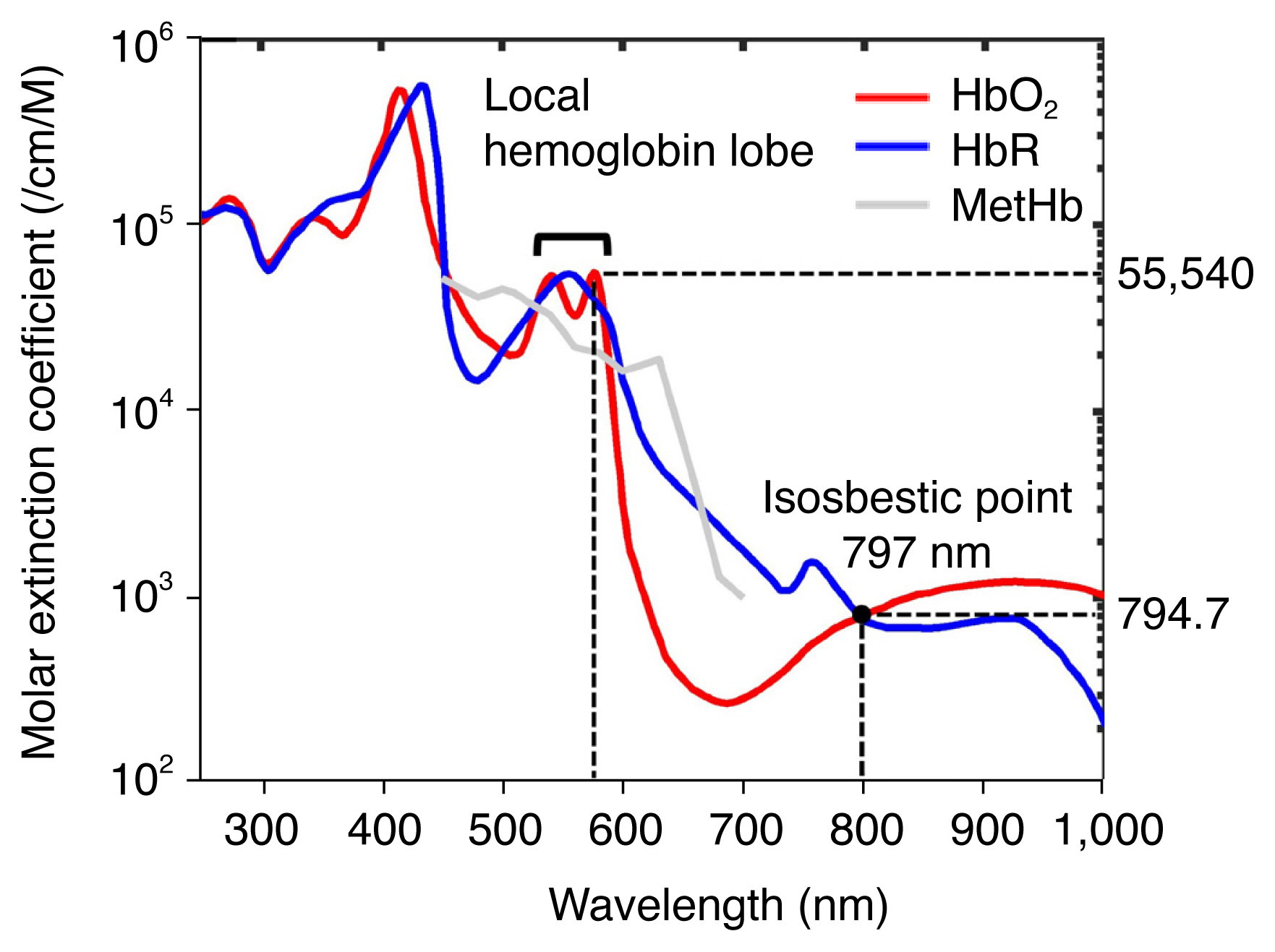 Fig. 1Experimental setup.
A. Thermal therapeutic setup was established using high-intensity focused ultrasound (HIFU). B. Spectroscopic photoacoustic (PA) imaging setup includes a piezoelectric linear array and optical fiber bundle. A translational XYZ stage was used to maneuver systems for precise scanning.
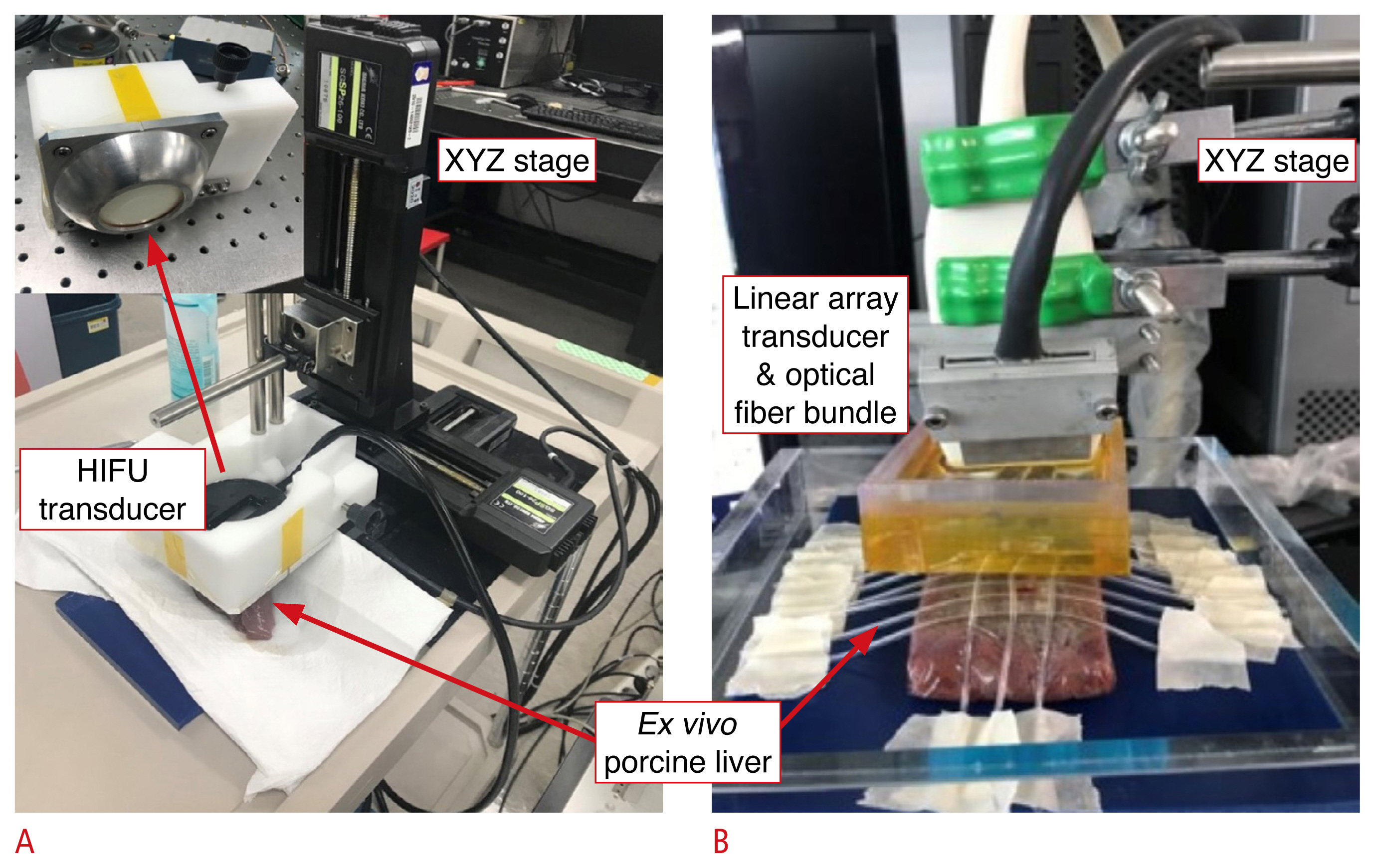 Fig. 2Thermal therapeutic characterization.
Temperature increases over time (A) and the corresponding CEM43 values (B) were measured and calculated, respectively. The red-shaded region indicates the effective CEM43 threshold for liver tissue ablation (
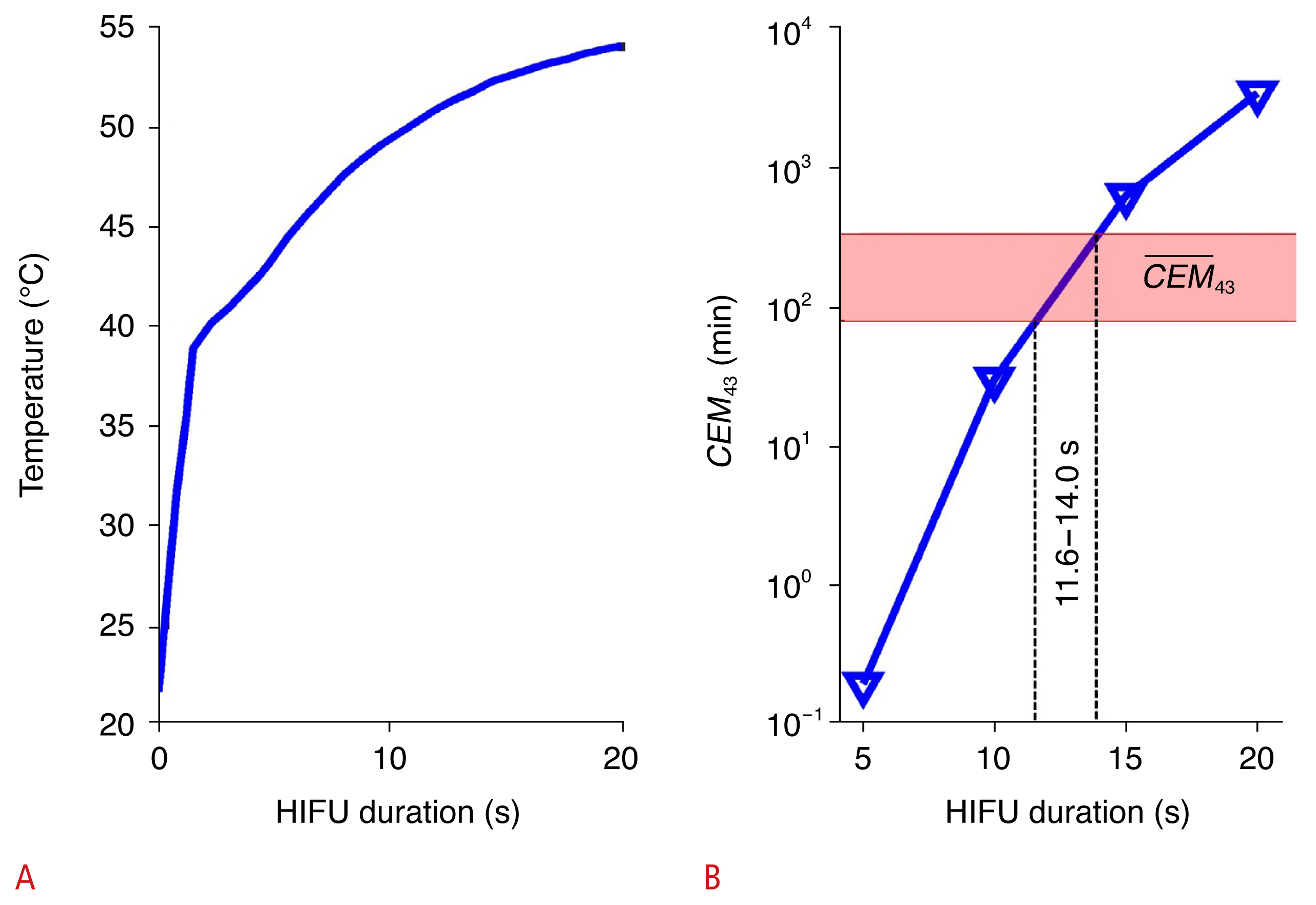 Fig. 3Spectral photoacoustic (PA) characterization during the thermal therapeutic process.
A. PA spectra in the visible wavelength range indicate different thermal therapeutic processes. Blue shades indicate the standard deviation at each wavelength (n=3). Black arrows emphasize the PA intensity dynamics in the range of thermal doses. Asterisks highlight the loss of the hemoglobin lobe at around 560 nm. B. Areas under the curve (AUC) of the PA spectra present different thermal therapeutic processes.
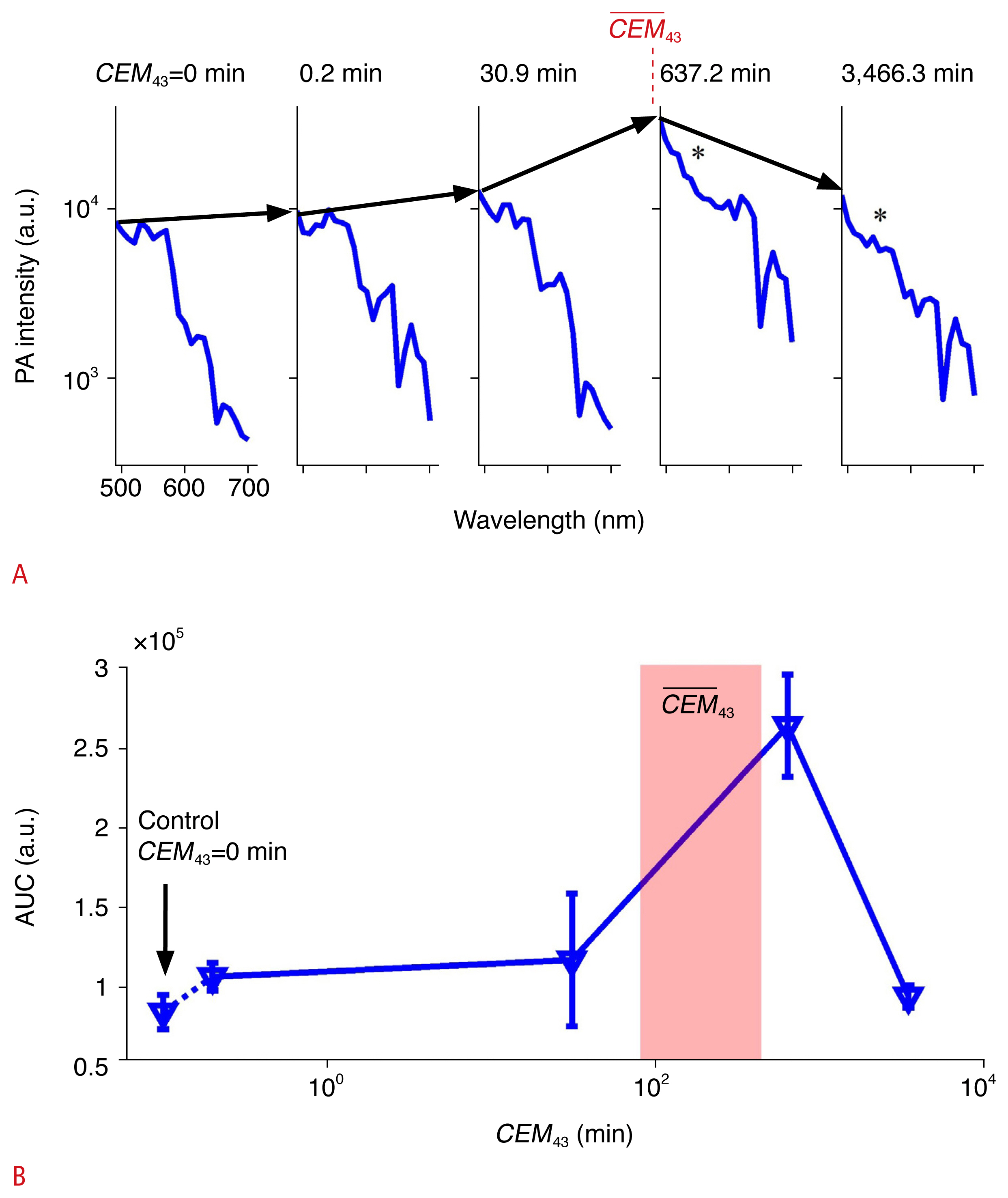 Fig. 4Calculation of the local hemoglobin lobe area.
A. Hemoglobin spectra were normalized at 510 nm to calculate the local hemoglobin lobe area. The dotted lines indicate the top of the baseline area between 510 nm and 600 nm. B. Local hemoglobin lobe area values were presented in a range of CEM43. The red shade indicates the
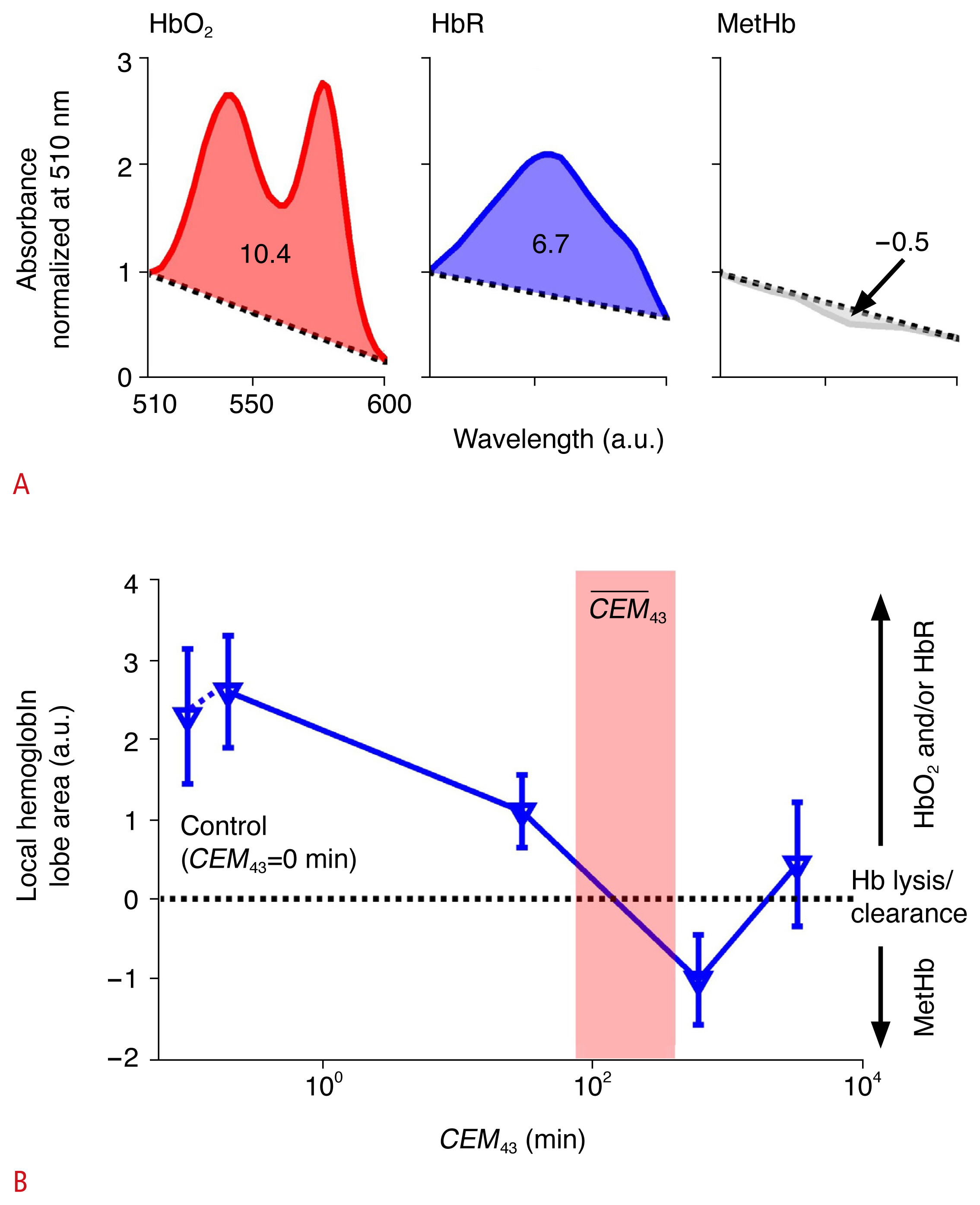 Fig. 5Hematoxylin and eosin–stained images to validate thermal ablation with different thermal doses in ex vivo porcine liver tissue.
A. ×200 magnification shows different thermal ablation processes when CEM43=0, 0.2, 30.9, 637.2, and 3,466.3 minutes. B. Images with ×400 magnification over black boxes in A indicate ablation when
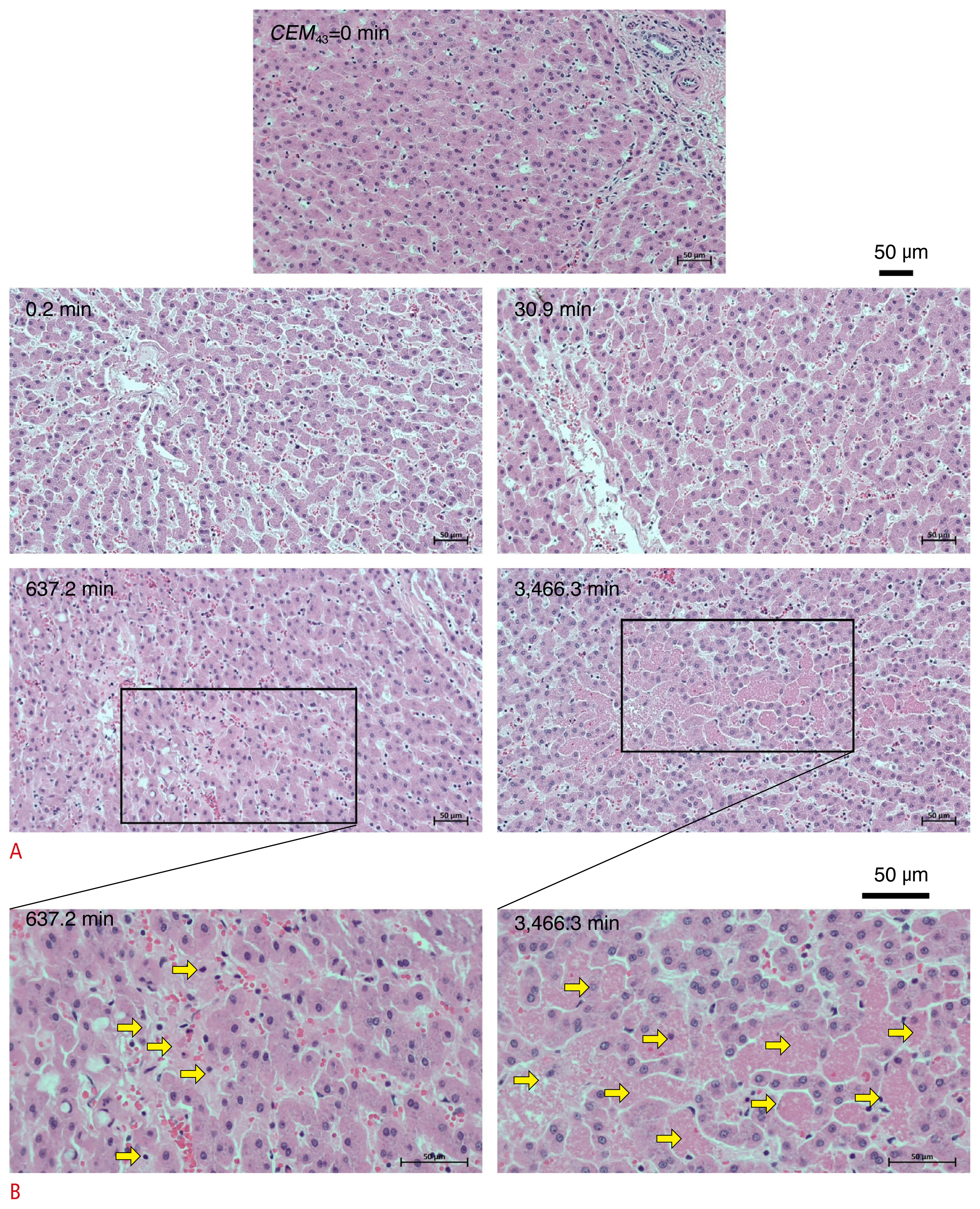 Fig. 6 |



 Print
Print facebook
facebook twitter
twitter Linkedin
Linkedin google+
google+
 Download Citation
Download Citation PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI




