Second-line Sonazoid-enhanced ultrasonography for Liver Imaging Reporting and Data System category 3 and 4 on gadoxetate-enhanced magnetic resonance imaging
Article information
Abstract
Purpose
This study investigated the utility of second-line contrast-enhanced ultrasonography (CEUS) using Sonazoid in Liver Imaging Reporting and Data System category 3 (LR-3) and 4 (LR-4) observations on gadoxetate-enhanced magnetic resonance imaging (MRI).
Methods
This retrospective study included LR-3 or LR-4 observations on gadoxetate-enhanced MRI subsequently evaluated with CEUS from 2013 to 2017. The presence of MRI features, CEUS-arterial phase hyperenhancement (CEUS-APHE), and Kupffer phase defect (KPD) was evaluated. Multivariable logistic regression analysis was performed to identify significant imaging features associated with the diagnosis of hepatocellular carcinoma (HCC). The optimal diagnostic criteria were investigated using the McNemar test.
Results
In total, 104 patients with 104 observations (63 HCCs) were included. The presence of both CEUS-APHE and KPD on CEUS enabled the additional detection of 42.3% (11/26) of LR-3 HCCs and 78.4% (29/37) of LR-4 HCCs. Transitional phase (TP) hypointensity (adjusted odds ratio [OR], 10.59; P<0.001), restricted diffusion (adjusted OR, 7.55; P=0.004), and KPD (adjusted OR, 7.16; P=0.003) were significant imaging features for HCC diagnosis. The presence of at least two significant imaging features was optimal for HCC diagnosis (sensitivity, specificity, and accuracy: 88.9%, 78.1%, and 84.6%, respectively), with significantly higher sensitivity than the presence of both CEUS-APHE and KPD (sensitivity, specificity, and accuracy: 63.5% [P=0.001], 92.7% [P=0.077], and 75.0% [P=0.089], respectively).
Conclusion
The combined interpretation of gadoxetate-enhanced MRI and second-line CEUS using Sonazoid, focusing on TP hypointensity, restricted diffusion, and KPD, may be optimal for further characterizing LR-3 and LR-4 observations.
Introduction
The Liver Imaging Reporting and Data System (LI-RADS), with the latest computed tomography (CT)/magnetic resonance imaging (MRI) diagnostic algorithm released in 2018, has become one of the major diagnostic tools for hepatocellular carcinoma (HCC) in at-risk patients [1,2]. LI-RADS categories 3 (LR-3) and 4 (LR-4) are designated for hepatic observations that have an intermediate probability of HCC or are probably HCC. The pooled proportions of HCC were as high as 31% and 64% in LR-3 and LR-4 observations, respectively, according to a recent meta-analysis [3], but observations in each category were heterogeneous in terms of HCC probability [4]. The suggested management options for LR-3 and LR-4 observations range from repeated or alternative diagnostic imaging within 3 to 6 months to a multi-disciplinary discussion for a tailored workup [2,5]. Immediate second-line diagnostic tests may further stratify HCC probability in these observations, enabling timely treatment of HCC.
The use of contrast-enhanced ultrasonography (CEUS) with a perfluorobutane microbubble agent (Sonazoid) is strongly recommended to diagnose HCC in observations with atypical enhancement patterns on CT or gadoxetate-enhanced MRI according to the Asian Pacific Association for the Study of the Liver (APASL) guidelines [6]. CEUS using Sonazoid, which is not yet included in CEUS LI-RADS [7], has a unique property for functional imaging as the contrast agent is phagocytosed by Kupffer cells [8]. A defect in the Kupffer phase obtained 10 minutes after contrast injection suggests a lack of normal functioning Kupffer cells within the observation [9]. Therefore, the Kupffer phase is useful for characterizing hepatic nodules in the process of hepatocarcinogenesis; whereas a Kupffer phase defect (KPD) favors the diagnosis of progressed HCC, iso-enhancement in the Kupffer phase indicates earlier stages of hepatocarcinogenesis [10-13].
In LI-RADS, hepatobiliary phase (HBP) hypointensity on gadoxetate-enhanced MRI is regarded as an ancillary feature favoring malignancy in general [14]. On gadoxetate-enhanced MRI, the majority of high-grade dysplastic nodules and early HCCs are categorized as LR-3 or LR-4, mainly attributable to HBP hypointensity [15]. Meanwhile, a KPD identified using CEUS with Sonazoid appears in a more advanced stage of hepatocarcinogenesis than HBP hypointensity [10,12,16]. In addition, CEUS with Sonazoid may detect tumor vascularity with the help of real-time imaging and defect-reperfusion imaging [17,18]. For these reasons, the APASL guidelines recommend Sonazoid CEUS for characterizing observations without arterial phase hyperenhancement (APHE) but with HBP hypointensity on gadoxetate-enhanced MRI, which are likely to be categorized as LR-3 or LR-4 on LI-RADS [6].
LI-RADS restricts the timing of washout to the portal venous phase on gadoxetate-enhanced MRI, but this may limit the sensitivity for HCC diagnosis [19,20]. However, the APASL guidelines may be limited by low specificity for the diagnosis of HCC because they allow hypointensity in HBP as an alternative to washout after exclusion of cavernous hemangioma [21,22]. Therefore, the combined use of second-line CEUS features and gadoxetate-enhanced MRI features may help overcome these limitations of both guidelines, and maximize the unique advantages of both imaging modalities.
The purpose of this study was to investigate the utility of second-line CEUS using Sonazoid in the characterization of LR-3 and LR-4 observations on gadoxetate-enhanced MRI.
Materials and Methods
Compliance with Ethical Standards
The study protocol was in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. The Institutional Review Board of Samsung Medical Center (approval number: 2019-08-026) approved this study and waived the requirement for patient consent as the study involved a retrospective review of medical records and images.
Patients
A review of medical records identified 543 potentially eligible patients with liver cirrhosis or chronic hepatitis B who underwent CEUS using Sonazoid for the evaluation of focal liver lesions from January 2013 to December 2017 at the authors’ institution. The inclusion criteria were patients with (1) gadoxetate-enhanced MRI obtained within 3 months before CEUS, and (2) LR-3 or LR-4 observations <30 mm on gadoxetate-enhanced MRI based on LI-RADS version 2018. If there were multiple observations in a patient, the largest observation was selected for the analysis. The exclusion criteria were (1) patients with inadequate CEUS or MRI quality, (2) subsequent treatment of the index lesion with ablation therapy or radiotherapy, (3) loss to follow-up after CEUS, and (4) lack of a reference standard. The indications for CEUS at the authors’ institution were (1) to characterize a lesion that was inconclusive on MRI, or (2) to increase the conspicuity of a lesion on ultrasonography to plan ablation therapy, upon request by referring physician.
There was a patient overlap with another study that compared the diagnostic performance of Sonazoid-enhanced CEUS and CT/MRI LI-RADS in LR-3, LR-4, LR-5, and LR-M lesions [23]. The present study investigated the added diagnostic value of Sonazoid-enhanced CEUS in LR-3 and LR-4 observations on MRI.
Image Acquisition
MRI scans were acquired using a 3.0-T system (Achieva, Philips Healthcare, Best, Netherlands). The routine protocol included dual-echo T1-weighted turbo field-echo images, breath-hold multi-shot T2-weighted images, respiratory-triggered single-shot heavily T2-weighted images, and respiratory-triggered single-shot echo-planar diffusion-weighted images with b-values of 0, 100, and 800 s/mm2 (Supplementary Table 1). For dynamic contrast-enhanced imaging, T1-weighted three-dimensional turbo field-echo images were obtained before and after the intravenous administration of gadoxetate disodium (Primovist, Bayer Healthcare, Berlin, Germany) using a power injector at a rate of 1 mL/s for a total dose of 0.025 mmol/kg body weight, followed by a 20 mL saline flush. The arterial phase, portal venous phase, transitional phase (TP), and HBP images were obtained approximately at 25-30 seconds, 60 seconds, 3 minutes, and 20 minutes after contrast injection; the arterial phase timing was determined using a magnetic resonance fluoroscopic bolus detection technique.
All CEUS examinations were performed by faculty-level abdominal radiologists with at least 10 years of clinical experience with CEUS. CEUS was performed with a 1-5 or 1-7 MHz convex probe using LOGIQ E9 (GE Healthcare, Milwaukee, WI, USA) or RS80A (Samsung Medison, Seoul, Korea) ultrasound systems. Ultrasound-MRI fusion was routinely performed by using Volume Navigation (GE Healthcare) or S-fusion (Samsung Medison) for accurate lesion localization, regardless of the conspicuity of the lesion on gray-scale ultrasonography. The MRI sequence that most clearly visualized each lesion and adjacent anatomic landmarks was selected for image fusion. After image fusion, CEUS was performed, with MRI being displayed side-by-side. Contrast harmonic imaging was used with a default mechanical index setting of 0.20 to 0.26. The beam focus was located at the posterior margin of the liver. A perfluorobutane microbubble agent (Sonazoid, GE Healthcare, Oslo, Norway) was administered at a dose of 0.015 mL/kg body weight by manual bolus injection via a peripheral venous line, followed by a 10 mL saline flush. Arterial phase, portal venous phase, late vascular phase, and postvascular phase (i.e., Kupffer phase) images were obtained approximately at 10-40 seconds, 60-90 seconds, 3-4 minutes, and 10 minutes after contrast injection, in agreement with the Asian Federation of Societies for Ultrasound in Medicine and Biology recommendations [24].
Image Analysis
A board-certified radiologist (Y.Y.K., with 6 years of experience in liver imaging) retrospectively evaluated the presence of major and ancillary features of the hepatic observations on MRI, including APHE (MR-APHE), washout, TP hypointensity, HBP hypointensity, mild to moderate T2 hyperintensity, and restricted diffusion, and assigned LI-RADS categories based on LI-RADS version 2018 [1]. In addition, the following CEUS features were retrospectively and independently evaluated by two board-certified radiologists (J.A.H. and J.H.M., with 9 and 11 years of experience in liver imaging, respectively): (1) APHE on CEUS (i.e., CEUS-APHE), defined as hyperenhancement in the arterial phase that is neither rim-like nor peripheral discontinuous globular enhancement, and (2) a KPD, defined as no enhancement or marked hypoenhancement to the liver in the Kupffer phase [24]. KPD was examined instead of CEUS washout because the current LI-RADS does not address the use of Sonazoid for CEUS, and the APASL guidelines recommend the use of KPD on second-line CEUS [6,7]. For observations with a nodule-in-nodule appearance, CEUS features of the inner nodule were recorded. Discrepancies between the two readers were resolved by another board-certified radiologist (W.K.J., with 20 years of experience in liver imaging), and the consensus reading results were used for data analysis. The radiologists were aware of the study purpose but were blinded to patients’ clinical information during image analysis. All images were reviewed using a picture archiving and communication system (Centricity Radiology RA 1000, GE Healthcare, Chicago, IL, USA).
Reference Standard
Electronic medical records and follow-up CT and/or MRI were reviewed to collect the reference standards. Observations were considered HCC if the lesion was pathologically diagnosed as HCC, or if compact Lipiodol uptake within the lesion was observed after transarterial chemoembolization [15,25,26]. Observations were considered benign if the lesion was pathologically diagnosed as benignancy, if the lesion resolved or was downgraded to LR-2 during follow-up, or if it remained stable for more than 24 months [27].
Statistical Analysis
Continuous variables were compared using the Student t-test or the Mann-Whitney U test, and categorical variables were compared using the chi-square test or the Fisher exact test according to the normality of the data distribution. Logistic regression analysis was performed to identify significant imaging features associated with HCC diagnosis. The backward elimination method was used to select variables for the multivariable analysis. Sensitivity, specificity, and accuracy for HCC were calculated for individual significant imaging features and their combinations, and comparisons were performed using the McNemar test. Subgroup analysis according to the LI-RADS category was performed. A two-sided P-value of less than 0.05 indicated statistical significance. The R package (version 3.6.1, The R Foundation for Statistical Computing, Vienna, Austria) was used for the analyses.
Results
Patient Characteristics
Of 543 potentially eligible patients, 350 patients met the inclusion criteria (Fig. 1). Of these, 20 patients who had CEUS or MRI of inadequate image quality, 169 patients who underwent subsequent treatment of index lesions with ablation therapy or radiotherapy, nine patients who were lost to follow-up after CEUS, and 48 patients who lacked a reference standard for the index lesion were excluded. Finally, 104 patients with 104 LR-3 or LR-4 observations were included.
Flow diagram of the study.
CEUS, contrast-enhanced ultrasonography; LR-3, Liver Imaging Reporting and Data System category 3; LR-4, Liver Imaging Reporting and Data System category 4; MRI, magnetic resonance imaging; Tx, treatment.
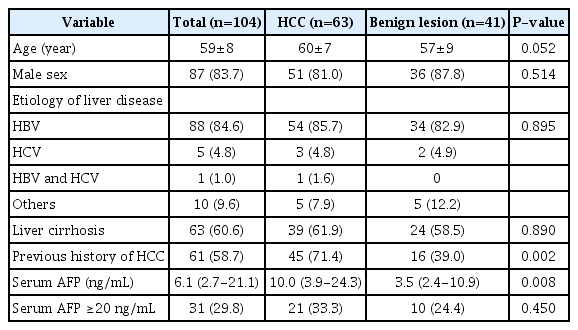
The clinical characteristics of 104 patients (mean age, 59±8 years [range, 34 to 78 years]; 87 men) are shown in Table 1. Eighty-nine patients (85.6%) had hepatitis B virus infections, and 63 patients (60.6%) had liver cirrhosis. Sixty-one patients (58.7%) had a prior history of HCC. Patients with HCC (n=63) more commonly had a history of HCC than those with benign lesions (n=41) (71.4% vs. 39.0%, P=0.002). Serum α-fetoprotein level was significantly higher in patients with HCC than those with benign lesions (median, 10.0 vs. 3.5 ng/mL, P=0.008), but the proportion of patients with the level ≥20 ng/mL was comparable (33.3% vs. 24.4%, P=0.450). The median time interval between MRI and CEUS was 13 days (interquartile range, 9 to 19 days).
Imaging Features According to Diagnosis
Sixty-three observations were diagnosed as HCC by pathologic proof (n=12; interval between MRI and reference standard, 0.3-5.9 months), or compact Lipiodol uptake after transarterial chemoembolization (n=51; 0.3-6.0 months). Forty-one observations were diagnosed as benignancy by pathologic proof (n=7; high-grade dysplastic nodule [n=1], low grade dysplastic nodule [n=1], regenerative nodule [n=1], focal nodular hyperplasia [n=2], and hemangioma [n=2]), or follow-up imaging (n=34).
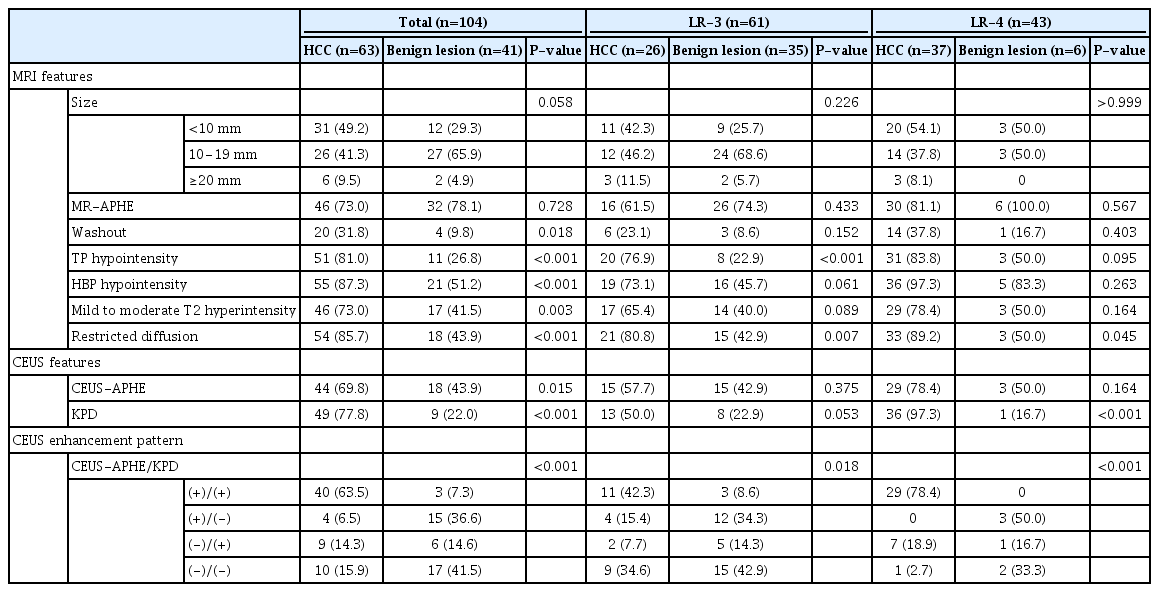
Washout (31.8% vs. 9.8%, P=0.018), TP hypointensity (81.0% vs. 26.8%, P<0.001), HBP hypointensity (87.3% vs. 51.2%, P<0.001), mild to moderate T2 hyperintensity (73.0% vs. 41.5%, P=0.003), restricted diffusion (85.7% vs. 43.9%, P<0.001), CEUS-APHE (69.8% vs. 43.9%, P=0.015), and KPD (77.8% vs. 22.0%, P<0.001) were more common in HCCs than in benign lesions (Table 2). The presence of both CEUS-APHE and KPD was more frequent in HCCs, and the absence of both CEUS-APHE and KPD was more common in benign lesions (Fig. 2).

Second-line CEUS features according to the diagnosis.
APHE, arterial phase hyperenhancement; CEUS, contrast-enhanced ultrasonography; HCC, hepatocellular carcinoma; KPD, Kupffer phase defect.
There were 61 (58.7%) LR-3 and 43 (41.3%) LR-4 observations (Table 2). The frequency of MR-APHE and CEUS-APHE were comparable in both LR-3 HCC (61.5% vs. 57.7%) and LR-4 HCC (81.1% vs. 78.4%), although three (11.5%) LR-3 HCCs, and five (13.5%) LR-4 HCCs showed APHE only on CEUS. However, eight (30.8%) LR-3 HCCs, and 23 (62.2%) LR-4 HCCs showed KPD in the absence of washout on MRI. In LR-3 subgroup, TP hypointensity was significantly less frequent in benign lesions (22.9% vs. 76.9%, P<0.001). In both LR-3 and LR-4 subgroups, restricted diffusion was more common in HCCs (LR-3, 80.8% vs. 42.9%, P=0.007; LR-4, 89.2% vs. 50.0%, P=0.045). In the LR-4 subgroup, KPD was significantly more frequent in HCC (97.3% vs. 16.7%, P<0.001), and the presence of both CEUS-APHE and KPD was only observed in HCCs (78.4% of LR-4 HCCs). The presence of both CEUS-APHE and KPD on second-line CEUS enabled the additional detection of 40 HCCs (42.3% [n=11] of LR-3 HCCs and 78.4% [n=29] of LR-4 HCCs) in LR-3 or LR-4 observations on MRI. Only three benign lesions showed CEUS-APHE and KPD in the LR-3 subgroup.
Logistic Regression Analysis
Multivariable analysis revealed that TP hypointensity (adjusted odds ratio [OR], 10.59; 95% confidence interval [CI], 2.96 to 37.89; P<0.001), restricted diffusion (adjusted OR, 7.55; 95% CI, 1.88 to 30.34; P=0.004), and KPD (adjusted OR, 7.16; 95% CI, 1.95 to 26.29; P=0.003) were independently associated with HCC diagnosis (Table 3). The adjusted OR for CEUS-APHE was 2.22 (95% CI, 0.67 to 7.39; P=0.194). Therefore, TP hypointensity, restricted diffusion, and KPD were identified as significant imaging features.
Performance of Significant Imaging Features for HCC Diagnosis
In all lesions, TP hypointensity (sensitivity and specificity, 81.0% and 73.2%, respectively) and KPD (sensitivity and specificity, 77.8% and 78.1%, respectively) showed the highest accuracy (77.9%) for HCC diagnosis among the significant imaging features (Table 4). The presence of at least two significant imaging features was optimal for HCC diagnosis (sensitivity, specificity, and accuracy of 88.9%, 78.1%, and 84.6%, respectively), with a significantly higher sensitivity than the presence of both CEUS-APHE and KPD (sensitivity, specificity, and accuracy of 63.5% [P=0.001], 92.7% [P=0.077], and 75.0% [P=0.089], respectively) (Fig. 3).

An 11-mm LR-4 observation in a 56-year-old man with hepatitis B virus-related liver cirrhosis and a prior history of HCC, which showed all significant imaging features and was pathologically diagnosed as HCC.
A, B. On gadoxetate-enhanced magnetic resonance imaging, the observation (arrow) shows no clear APHE (MR-APHE) (A) or washout (B). C, D. The observation (arrow) shows transitional phase hypointensity (C), hepatobiliary phase hypointensity (not shown), mild to moderate T2 hyperintensity (not shown), and restricted diffusion on b=800 s/mm2 image (D). E, F. On second-line CEUS performed 24 days later, CEUS-APHE (E) and Kupffer phase defect (arrow) are demonstrated (F). LR-4, Liver Imaging Reporting and Data System category 4; HCC, hepatocellular carcinoma; APHE, arterial phase hyperenhancement; CEUS, contrast-enhanced ultrasonography.
In the LR-3 subgroup, TP hypointensity had the highest accuracy (77.1%) with sensitivity and specificity of 76.9% and 77.1%, respectively (Fig. 4). In the LR-4 subgroup, KPD had the highest accuracy (95.4%), with sensitivity and specificity of 97.3% and 83.3%, respectively. The performance measures of the optimal criteria (the presence of at least two significant imaging features) were comparable to those of TP hypointensity in the LR-3 subgroup, and to those of KPD in the LR-4 subgroup (all P-values >0.999).
A 15-mm LR-3 observation in a 65-year-old man with liver cirrhosis of unknown etiology and a prior history of hepatocellular carcinoma, which showed no significant imaging features and was finally determined to be benign.
A. On the index gadoxetate-enhanced MRI, the observation (arrow) shows arterial phase hyperenhancement but no washout or ancillary features favoring malignancy (not shown). B, C. On contrast-enhanced ultrasonography using Sonazoid performed 11 days later, the observation is isoechoic to the liver in the arterial phase (B) and the Kupffer phase (C). D. On gadoxetate-enhanced MRI taken 25 months after the index MRI, the observation (arrow) remains unchanged in size and characteristics. LR-3, Liver Imaging Reporting and Data System category 3; MRI, magnetic resonance imaging.
Discussion
In this study, the value of second-line CEUS with Sonazoid for the diagnosis of HCC was retrospectively analyzed in LR-3 and LR-4 observations on gadoxetate-enhanced MRI. It is notable that the presence of both CEUS-APHE and KPD on second-line CEUS enabled the additional detection of 63.5% of HCCs in this study. The sensitivity for HCC was 42.3% in the LR-3 subgroup and 78.4% in the LR-4 subgroup, with high specificity (91.4% in the LR-3 subgroup and 100.0% in the LR-4 subgroup). Furthermore, the combined use of second-line CEUS features and gadoxetate-enhanced MRI features showed the optimal diagnostic performance for HCC by improving the sensitivity for HCC to 88.9%. The presence of at least two significant imaging features (TP hypointensity, restricted diffusion, and KPD) showed a sensitivity of 76.9% in the LR-3 subgroup and 97.3% in the LR-4 subgroup. Although second-line CEUS showed additional diagnostic value in LR-3 and LR-4 observations with high specificity, the combined interpretation of MRI and CEUS enabled the better detection of HCC in these lesions.
The results of the present study suggest that second-line Sonazoid CEUS could be a viable alternative diagnostic imaging option in LR-3 and LR-4 observations [2,5]. The APASL guidelines highly recommend that second-line CEUS with Sonazoid should be used to diagnose HCC in observations that do not show MR-APHE but depict HBP hypointensity on gadoxetate-enhanced MRI [6]. This study expanded the APASL indication to LR-3 or LR-4 observations, and showed a promising diagnostic performance for HCC. Of note, lack of washout on gadoxetate-enhanced MRI was one of the major reasons for HCC to be categorized as LR-3 or LR-4 on MRI. In the LR-4 subgroup, KPD provided a diagnosis that was both highly sensitive and highly specific, and the presence of both CEUS-APHE and KPD was only observed in HCC in the LR-4 subgroup. Prior studies have suggested that KPD is more specific to progressed HCC than HBP hypointensity [10,12,16]. According to another study [13], Kupffer phase iso-enhancement, especially when CEUS-APHE is absent, rarely indicated HCC, which is in agreement with the present study results. Considering that KPD showed comparable diagnostic performance to the optimal criteria in the LR-4 subgroup, a second-line diagnostic workup using Sonazoid CEUS can be especially necessary for LR-4 observations.
However, the incremental value of CEUS-APHE was somewhat smaller than expected. A recent study using a purely intravascular CEUS agent showed a comparable frequency of CEUS-APHE and MR-APHE (77.7% vs. 72.8%) in LR-3, LR-4, LR-5, and LR-M observations [28]. In this study using Sonazoid, approximately 10% of HCCs showed APHE only on CEUS, not on MRI. Although CEUS may display APHE in some cases in which gadoxetate-enhanced MRI fails to capture APHE [29], the added value of CEUS-APHE may not be substantial, as shown by the results of multivariable logistic regression analysis in the present study. Nonetheless, CEUS-APHE was significantly less frequent in benign lesions than in HCCs (43.9% vs. 69.8%), suggesting that it may be more specific than MR-APHE benign lesion vs. HCC (78.1% vs. 73.0%).
The combined interpretation of gadoxetate-enhanced MRI and second-line CEUS was optimal rather than using CEUS features alone. Interestingly, ancillary features favoring malignancy in the LI-RADS diagnostic algorithm, such as TP hypointensity and restricted diffusion, were designated as significant imaging features. TP hypointensity may help overcome the limitation of portal venous phase washout on gadoxetate-enhanced MRI [19]. In addition, restricted diffusion is regarded as an indicator of progressed HCC in comparison with early HCC or dysplastic nodules [30,31]. These features have also been emphasized as key ancillary features of LI-RADS [4,32,33]. The optimal diagnostic criteria identified herein may be a useful strategy for applying ancillary MRI features to LR-3 and LR-4 observations.
This study has some limitations. First, selection bias may have been introduced by retrospectively analyzing observations that were evaluated both with MRI and CEUS. Further studies with a prospective study design are warranted to overcome this limitation and strengthen the results. Second, the diagnostic value of portal venous phase or late vascular phase CEUS images was not evaluated, but warrants further investigation. Third, inter-operator variability in CEUS examinations may have existed. However, the variability would be small, as ultrasound-MRI fusion was routinely performed to enable accurate localization of observations noted on MRI. Fourth, the majority (85.6%) of patients had hepatitis B virus infection, which may limit the generalizability of the results.
In conclusion, second-line CEUS with Sonazoid can additionally detect HCC in LR-3 or LR-4 observations on gadoxetate-enhanced MRI with excellent specificity. Combined interpretation of MRI and CEUS, with a focus on TP hypointensity, restricted diffusion, and KPD, may be an optimal strategy for further characterizing LR-3 and LR-4 observations on gadoxetate-enhanced MRI.
Notes
Author Contributions
Conceptualization: Min JH, Jeong WK, Shin DH, Lim HK. Data acquisition: Kim YY, Min JH, Hwang JA, Jeong WK. Data analysis or interpretation: Kim YY, Min JH, Hwang JA, Jeong WK, Shin DH, Lim HK. Drafting of the manuscript: Kim YY. Critical revision of the manuscript: Min JH, Hwang JA, Jeong WK, Shin DH, Lim HK. Approval of the final version of the manuscript: all authors.
No potential conflict of interest relevant to this article was reported.
Supplementary Material
Supplementary Table 1.
MRI parameters (https://doi.org/10.14366/usg.21198).
References
Article information Continued
Notes
Key point
Transitional phase (TP) hypointensity, restricted diffusion, and Kupffer phase defect (KPD) were independently associated with hepatocellular carcinoma (HCC) diagnosis in Liver Imaging Reporting and Data System category 3 (LR-3) and category 4 (LR-4) observations. The presence of both contrast-enhanced ultrasonography (CEUS) arterial phase hyperenhancement and KPD on second-line CEUS could additionally detect 42.3% of LR-3 HCCs and 78.4% of LR-4 HCCs, and the enhancement pattern was only observed in HCCs in the LR-4 subgroup. Combined interpretation of magnetic resonance imaging and second-line CEUS using at least two significant imaging features (TP hypointensity, restricted diffusion, and KPD) was optimal for diagnosing HCC.