Subcategorization of intermediate suspicion thyroid nodules based on suspicious ultrasonographic findings
Article information
Abstract
Purpose
This study compared the malignancy risk of intermediate suspicion thyroid nodules according to the presence of suspicious ultrasonographic (US) findings.
Methods
From January 2014 to December 2014, 299 consecutive intermediate suspicion thyroid nodules in 281 patients (mean age, 50.6±12.5 years) with final diagnoses were included in this study. Two radiologists retrospectively reviewed the US findings and subcategorized the intermediate suspicion category into nodules without suspicious findings and nodules with suspicious findings, including punctate echogenic foci, nonparallel orientation, or irregular margins. The malignancy rates were compared between the two subcategory groups.
Results
Of the 299 intermediate suspicion thyroid nodules, 230 (76.9%) were subcategorized as nodules without suspicious findings and 69 (23.1%) as nodules with suspicious findings. The total malignancy rate was 33.4% (100/299) and the malignancy rate of nodules with suspicious findings was significantly higher than that of nodules without suspicious findings (47.8% vs. 29.1%, P=0.004). In nodules with suspicious findings, the most common suspicious finding was punctate echogenic foci (48/82, 58.5%) followed by nonparallel orientation (22/82, 26.8%) and irregular margins (12/82, 14.6%). Thirteen nodules had two suspicious findings simultaneously. A linearly increasing trend in the malignancy rate was observed according to the number of suspicious US findings (P for trend=0.001).
Conclusion
Intermediate suspicion thyroid nodules with suspicious findings showed a higher malignancy rate than those without suspicious findings. Further management guidelines for nodules with suspicious findings should differ from guidelines for nodules without suspicious findings, even in the same US category.
Introduction
Advances in high-resolution ultrasonography (US) have resulted in a high prevalence of thyroid incidentalomas; however, most nodules are benign [1]. To guide physicians in the proper management of thyroid nodules, several international guidelines have been developed, and US-based risk stratification has been suggested to aid in deciding when to perform fine-needle aspiration (FNA) or recommend follow-up US for thyroid nodules [2-9]. Several studies have compared the diagnostic performance of various US-based risk stratification systems for diagnosing thyroid malignancies and revealed that the Korean Thyroid Imaging Reporting and Data System (K-TIRADS), proposed by the Korean Society of Thyroid Radiology/Korean Thyroid Association, had higher sensitivity than other systems [10-14]. Nonetheless, the studies also reported that the rate of unnecessary biopsies was higher in K-TIRADS, which had lower specificity [10-15]. As part of an effort to reduce unnecessary biopsies, some studies have simulated different size cutoffs for biopsies and revealed that the higher rate of unnecessary biopsies of K-TIRADS is attributed to the lower cutoff sizes for biopsies [11,16,17].
The malignancy risk of K-TIRADS category 4 (intermediate suspicion thyroid nodules) spans a relatively wide range, from 10% to 40% [9]. This category encompasses nodules with various US findings, including (1) solid hypoechoic nodules without any of three suspicious US features (i.e., punctate echogenic foci, nonparallel orientation, or irregular margins), (2) entirely calcified nodules, and (3) partially cystic or isoechoic/hyperechoic nodules with any of the three aforementioned suspicious US features [9]. Meanwhile, the recently revised 2021 K-TIRADS suggests that the cutoff size for FNA should be determined within the range of 1 and 1.5 cm, based on the US features, nodule location, clinical risk factors, and patient factors (age, co-morbidities, and preferences) or more, collectively [9]. Na et al. [16] recently published a study on a modification of K-TIRADS, wherein intermediate suspicion nodules were subcategorized into 4A and 4B based on the malignancy risk of US patterns according to the previous 2016 K-TIRADS. This was based on previous studies reporting that the degree of hypoechogenicity, macrocalcification, and a higher number of suspicious US features are associated with an increased malignancy risk [18-20]. The malignancy rate was different in the two subgroups, so the authors suggested different biopsy thresholds to reduce unnecessary biopsies [16].
Starting from a similar concept, the present study aimed to divide intermediate suspicion thyroid nodules into two different subgroups according to the revised 2021 K-TIRADS, focusing on the presence of suspicious US features, and to investigate whether the malignancy rate is different between these two subgroups.
Materials and Methods
Compliance with Ethical Standards
This retrospective study was approved by the Institutional Review Board of Samsung Medical Center (IRB No. 2021-06-027) the author’s affiliated institution, and the requirement for informed consent was waived. However, informed consent for FNA or core needle biopsy (CNB) had been obtained from all patients before the procedure.
Study Population
Consecutive patients who underwent thyroid FNA or CNB at single tertiary hospital between January 2014 and December 2014 were enrolled in this study. During this period, 338 thyroid nodules ≥1 cm were classified into the intermediate suspicion category on US, of which FNA was performed for 252 nodules and CNB for 86 nodules. Among 252 FNA cases, 21 were excluded owing to the absence of a final diagnosis. Among 86 CNB cases, 18 were excluded because no final diagnosis was present. We finally included 299 intermediate suspicion thyroid nodules ≥1 cm (mean size, 2.1±1.1 cm; range, 1.0 to 6.7 cm) in 281 patients (mean age, 50.6±12.5 years; range, 18 to 80 years).
Final Diagnosis
The final diagnoses of malignant tumors were determined by (1) surgical pathology or (2) a malignant result on CNB. The final diagnoses of benign nodules were determined by (1) pathological results of surgical resections or (2) concordant US imaging findings with a benign FNA or CNB result, with or without follow-up [21,22].
US Examinations and US Image Analyses
All thyroid US examinations were performed with a 5-12 MHz linear array transducer (iU22, Philips Medical Systems, Bothell, WA, USA) by one of 11 radiologists (nine faculty members and two fellows) with 1-18 years of experience in thyroid imaging. Two radiologists (S.Y.H. and H.K., with 14 and 2 years in thyroid imaging) retrospectively reviewed the US images in consensus. Each nodule was categorized based on the US features according to the revised 2021 K-TIRADS [9]. All thyroid nodules were evaluated for composition, echogenicity, orientation, margin, and echogenic foci. The composition was categorized as solid (no obvious cystic component), predominantly solid (≤50% of the cystic portion), predominantly cystic (>50% of the cystic portion), cystic (no obvious solid content), or spongiform (microcystic changes >50% of the solid component). The echogenicity was categorized as markedly hypoechoic, mildly hypoechoic, isoechoic, or hyperechoic. The orientation was classified as parallel or nonparallel. The margin was classified as irregular, smooth, or ill-defined. If echogenic foci were present, they were classified as punctate echogenic foci (echogenic foci ≤1 mm within the solid component), macrocalcifications (echogenic foci >1 mm with posterior shadowing), or as complete or incomplete rim calcification (peripheral curvilinear hyperechoic line surrounding the nodule margin with or without posterior shadowing). Thyroid nodules with the following US findings were categorized into K-TIRADS category 4 (intermediate suspicion nodules): (1) solid hypoechoic nodules without any of the three suspicious US features (i.e., punctate echogenic foci, nonparallel orientation, or irregular margins), (2) entirely calcified nodules, or (3) partially cystic or isoechoic/hyperechoic nodules with any of the three aforementioned suspicious US features. Intermediate suspicion thyroid nodules were divided into two different subgroups: nodules without suspicious US findings and nodules with suspicious findings.
Statistical Analyses
All categorical variables were analyzed using the chi-square or Fisher exact test, and continuous variables were assessed using the Student t-test. The Cochran-Armitage test for trend was used to evaluate the linear trend between the number of suspicious findings and the malignancy rate. Analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). All tests were two-sided, and a P-value of <0.05 was considered indicative of a statistically significant difference.
Results
Of a total of 299 intermediate suspicion nodules, 230 (76.9%) had no suspicious findings and 69 (23.1%) had suspicious findings. Table 1 summarizes the clinicopathologic characteristics of the patients and nodules. There were no significant differences in age, sex, and tumor size between the two groups (P=0.871, P=0.056, and P=0.905, respectively). The most common result of FNA or CNB was benign (Bethesda or CNB diagnostic category II) in both groups. However, the second most common result of FNA or CNB was follicular neoplasm/suspicious for follicular neoplasm (Bethesda or CNB diagnostic category IV) in nodules without suspicious findings (17.0%), and malignant (Bethesda or CNB diagnostic category VI) in nodules with suspicious findings (23.2%). The malignant category (Bethesda or CNB diagnostic category VI) was significantly more frequent in nodules with suspicious findings than in nodules without suspicious findings (23.2% vs. 9.6%, P=0.003). The frequency of follicular neoplasm/suspicious for follicular neoplasm (Bethesda or CNB diagnostic category IV) was not significantly different between the two groups (P=0.933). The most common final diagnosis was benign follicular nodule in both groups (97 of 230 [42.2%] and 24 of 69 [34.8%], respectively). Follicular adenoma (38 of 230 [16.5%]) was the second most common result of final diagnosis in nodules without suspicious findings (Fig. 1) and classic papillary thyroid carcinoma (PTC) (19 of 69 [27.5%]) was the second most common final diagnosis in nodules with suspicious findings. Although the follicular variant of PTC (28 of 67 [41.8%]) was the most frequent final malignant diagnosis of nodules without suspicious findings and classic PTC (19 of 33 [57.6%]) (Fig. 2) was the most frequent final malignant diagnosis of nodules with suspicious findings, the difference was not statistically significant (P=0.246). There was also no lymphoma or metastasis in the nodules with suspicious findings, while three of the nodules without suspicious findings were lymphoma and one was metastasis.
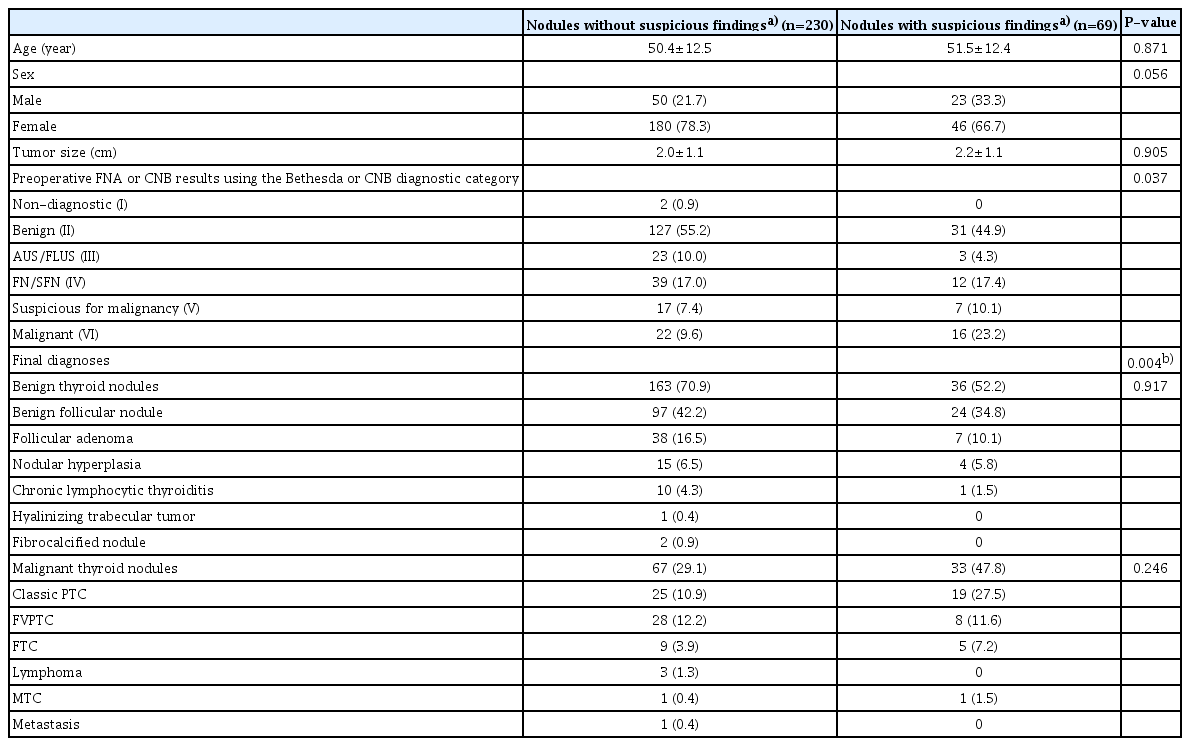
Clinicopathologic characteristics of the two subcategories of intermediate suspicion thyroid nodules (K-TIRADS 4)
A 41-year-old woman with an intermediate suspicion nodule without suspicious findings in the left thyroid lobe.
Transverse (A) and longitudinal (B) ultrasonography show a 2.6-cm solid nodule with hypoechogenicity, smooth margin, and without any suspicious ultrasonograpic features. The result of ultrasonography-guided core needle biopsy was suspicious for follicular neoplasm (Bethesda category IV). The nodule was confirmed as a follicular adenoma after surgery.
A 26-year-old woman with an intermediate suspicion nodule with suspicious findings in the left thyroid lobe.
Transverse (A) and longitudinal (B) ultrasonography show a 1.9-cm predominantly solid nodule with isoechogenicity, irregular margins, nonparallel orientation, and punctate echogenic foci. The result of ultrasonography-guided fine-needle aspiration was malignancy (Bethesda category VI). The nodule was confirmed as a papillary thyroid carcinoma after surgery.
The total malignancy rate was 33.4% (100/299), and the malignancy rate was significantly higher in nodules with suspicious findings than in nodules without suspicious findings (47.8% vs. 29.1%, P=0.004). When the nodules were grouped into nodules without suspicious findings, nodules with one suspicious finding, and nodules with two suspicious findings, the malignancy rate was significantly different across the number of suspicious US findings (P<0.001), and a linearly increasing trend was observed in those three subgroups of intermediate suspicion nodules (P for trend=0.001) (Table 2). Among 230 nodules without suspicious findings, 18 were entirely calcified nodules, and 38.9% of them (7/18) were malignant (Fig. 3). Of 212 nodules without suspicious findings excluding entirely calcified nodules, 28.3% (60/212) were malignant.
A 61-year-old woman with an intermediate suspicion nodule without suspicious findings in the left thyroid lobe.
Transverse (A) and longitudinal (B) ultrasonography show a 1.4-cm entirely calcified nodule. The result of ultrasonography-guided fine-needle aspiration was benign (Bethesda category II). The nodule was confirmed as a fibrocalcified nodule after surgery.
The most common suspicious US feature in nodules with suspicious findings was punctate echogenic foci (48/82, 58.5%), followed by nonparallel orientation (22/82, 26.8%) and irregular margins (12/82, 14.6%). Thirteen nodules had two suspicious findings simultaneously. In nodules with suspicious findings, nodules with punctate echogenic foci only were the most frequent (37/69, 53.6%), followed by nodules with nonparallel orientation only (14/69,20.3%), and nodules with punctate echogenic foci and nonparallel orientation (6/69, 8.7%) (Table 3). The malignancy rate was not significantly different between nodules with one suspicious finding and nodules with two suspicious findings (42.9% [24 of 56] vs. 69.2% [9 of 13], P=0.086).
Discussion
This study investigated the malignancy rate of two subcategories of K-TIRADS category 4 (intermediate suspicion nodules) and revealed that nodules with any of the three suspicious US findings showed a significantly higher malignancy rate than nodules without suspicious findings. A previous study divided K-TIRADS 4 nodules into two subgroups and reported different malignancy rates in each subcategory [16]. Unlike the present study, those researchers considered the combination of the degree of hypoechogenicity, the presence of macrocalcification, and the number of suspicious US features according to the previous 2016 K-TIRADS, while the present study simply considered the presence of suspicious US findings and applied the revised 2021 K-TIRADS. Despite an increasing trend in the malignancy rate according to the number of suspicious US findings, there was no significant difference in the malignancy rate between nodules with one suspicious finding and nodules with two suspicious findings in this study (P=0.086). However, the main conclusion was the same—namely, the malignancy rate differed in the K-TIRADS 4 subcategory according to the US findings.
Oval circumscribed benign nodules observed with diffuse thyroid disease, which might have been interpreted as isoechoic low-suspicion nodules according to the 2016 K-TIRADS, may have been classified as nodules without suspicious findings in this study, as nodule echogenicity is defined relative to the presumed normal thyroid echogenicity instead of the surrounding parenchymal echogenicity according to the revised 2021 K-TIRADS [4,9]. This might be a reason explaining the higher benignity of the nodules without suspicious findings.
The revised 2021 K-TIRADS, which was recently released, suggested that the size threshold for FNA of K-TIRADS 4 nodules should be determined within the range of 1 and 1.5 cm, based on the US features, nodule location, clinical risk factors, and demographic factors such as age, co-morbidities, and preferences [9]. This range was based on precedent studies of the modified K-TIRADS that showed a significantly reduced unnecessary biopsy rate for small thyroid nodules (1-2 cm), while maintaining a very high sensitivity for large nodules (>2 cm) [17,23]. For practical and clinical applications, however, there may be ambiguous or confusing cases with the proposed range of the biopsy size threshold. In that context, the results of this study might help in determining whether to biopsy K-TIRADS 4 nodules sized between 1 to 1.5 cm, insofar as histologic confirmation by FNA or CNB could be more preferred for nodules with suspicious US findings than for nodules of the same size without suspicious US findings.
This study had limitations. First, the reproducibility of the US findings might have been operator-dependent, especially in this retrospective study. However, a previous study reported equal inter-examination agreement between retrospective and real-time US image interpretation for thyroid nodules using the K-TIRADS [24]. Second, selection bias might have occurred as all patients were recruited at a single tertiary referral center. This might have led to an overestimation of the malignancy rate.
In conclusion, as two subcategories of intermediate suspicion thyroid nodules clearly showed different malignancy rates, further management guidelines should be different between the two subgroups. When determining whether to perform biopsy for an intermediate suspicion nodule based on the revised 2021 K-TIRADS, the presence or absence of suspicious US findings including punctate echogenic foci, nonparallel orientation, or irregular margins can also be considered—specifically, a biopsy may be attempted in smaller nodules with suspicious US findings than in nodules without suspicious US findings, within the suggested size range of 1 cm to 1.5 cm.
Notes
Author Contributions
Conceptualization: Kim H, Hahn SY. Data acquisition: Kim H, Hahn SY, Shin JH, Kim KE, Kim MK, Oh J. Data analysis or interpretation: Hahn SY, Shin JH, Kim KE, Kim MK, Oh J. Drafting of the manuscript: Kim H, Hahn SY, Kim KE, Kim MK. Critical revision of the manuscript: Kim H, Hahn SY, Shin JH, Oh J. Approval of the final version of the manuscript: all authors.
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Key point
Intermediate suspicion thyroid nodules with suspicious ultrasonographic (US) findings showed a higher malignancy rate than nodules without suspicious US findings. Further management guidelines for intermediate suspicion nodules should differ according to the presence of suspicious US findings even within the same US category.


