Evaluation of cervical lymph node metastasis in thyroid cancer patients using real-time CT-navigated ultrasonography: preliminary study
Article information
Abstract
Purpose:
To evaluate the diagnostic accuracy of real-time neck computed tomography (CT)-guided ultrasonography (US) in detecting cervical neck lymph node metastasis (LNM) in patients with papillary thyroid cancer (PTC).
Methods:
We retrospectively reviewed data from 176 patients (mean age, 43 years; range, 23 to 74 years) with surgically confirmed PTC who underwent preoperative US, neck CT, and neck CTguided US. We then compared the sensitivities and diagnostic accuracies of each of the three above modalities in detecting cervical LNM.
Results:
Preoperative US showed 17.3% sensitivity and 58.5% diagnostic accuracy in detecting central LNM compared with 64.3% sensitivity and 89.2% diagnostic accuracy in detecting lateral neck LNM. Neck CT showed 23.5% sensitivity and 55.7% diagnostic accuracy in detecting central LNM and 71.4% sensitivity with 90.9% diagnostic accuracy in detecting lateral neck LNM. CT-guided US exhibited 37.0% sensitivity and 63.1% diagnostic accuracy in detecting central LNM compared with 92.9% sensitivity and 96.0% diagnostic accuracy in detecting lateral LNM. CT-guided US showed higher diagnostic accuracy with superior sensitivity in detecting central and lateral LNM than did US (P<0.001, P=0.011) and CT (P=0.026, P=0.063).
Conclusion:
Neck CT-guided US is a more accurate technique with higher sensitivity for detecting cervical LNM than either US or CT alone. Therefore, our data indicate that neck CT-guided US is an especially useful technique in preoperative examinations.
Introduction
Ultrasonography (US) and neck computed tomography (CT) are used for diagnosing papillary thyroid cancer (PTC) in many institutions. US is the main preoperative imaging technique since it is better able to characterize malignant features of the thyroid nodule due to the high resolution of US images, which have been shown to be able to detect metastatic lymph nodes (LNs) as small as 5 mm in diameter [1]. The preoperative use of neck CT is not routinely recommended in the American Thyroid Association management guidelines [2]. However, US is operator-dependent and it is often difficult to obtain adequate US images of the entire neck [3,4]. Contrastingly, neck CT is nonoperator dependent and allows complete LN assessments of the entire neck. Therefore, in practice, neck CT is frequently used for detecting cervical lymph node metastasis (LNM).
Recently, a fusion imaging system has been applied to realtime US for the evaluation of various organs in order to improve diagnostic performance. However, no published studies have analyzed the application of the fusion imaging system in thyroid cancer. We conducted this study to evaluate the sensitivity and diagnostic accuracy of real-time neck CT-guided US for detecting cervical LNM in patients with PTC.
Materials and Methods
Patients
Our retrospective study was approved by the Institutional Review Board of our institution. Informed consent was not required for the review of patient medical records, US images, or CT images.
The study population consisted of 176 patients with surgically proven PTCs who underwent preoperative US, neck CT, and CTguided US at Kangbuk Samsung Hospital (Seoul, Korea). The PTCs were confirmed by US-guided fine needle aspiration before cancer staging was performed. Preoperative US, neck CT, and CT-guided US were performed and reported independently for the staging workup. Each of the patients underwent surgery for thyroid papillary cancer within one month of the preoperative exam. The patients were treated between March 1, 2011, and February 3, 2012. All patients underwent a postoperative US or positron emission tomography (PET) CT scan 9 months (range, 6 to 15 months) after surgery to evaluate local recurrence or distant metastasis.
In total, 176 patients with PTC underwent surgery. Of these 176 patients, 59 (33.5%) underwent a hemithyroidectomy with ipsilateral central neck lymph node dissection (LND), 93 (52.8%) underwent a total thyroidectomy with bilateral central LND, and 24 (13.6%) patients underwent a total thyroidectomy with central and lateral LND. All central and lateral LNs that appeared suspicious in US, neck CT, or CT-guided US were dissected. We defined patients who did not undergo lateral LND as negative when follow-up PET CT scans showed negative results for LNM or when postoperative follow-up US scans were negative.
Preoperative Image Study
The presence of central and lateral LNM was evaluated in patients who subsequently underwent surgery for PTC. In each case, three board-certified radiologists with three to ten years of experience in thyroid US performed preoperative US examinations of thyroid lesions and cervical LNs. Examinations were performed with a Logiq E9 apparatus (Volume Navigation, General Electric, Milwaukee, WI, USA) equipped with a high-frequency 13 MHz linear transducer. multi-detector CT (MDCT) images of the neck were also obtained before the surgery and were interpreted by two head and neckspecialized radiologists with more than ten years of experience who did not perform the US and CT-guided US. MDCT images were captured with a BRILLIANCE 190p 40-channel unit (Philips Medical System, Best, The Netherlands). Scans were obtained with a reconstructed slice thickness of 3 mm for unenhanced, enhanced axial, and enhanced coronal images, and the helical pitch was 0.6. For contrast-enhanced studies, 120 mL of a nonionic contrast medium (300 mg/mL Omnipaque, GE Healthcare, Oslo, Norway) was administered at an injection rate of 3 mL/sec. The scan delay for contrast-enhanced images was 60 seconds. For correlative analysis of LN results according to CT and US, the neck was divided into two compartments: the central compartment, which encompassed the region between the medial margins of the bilateral carotid arteries (including level VI), and the lateral compartment, which encompassed the region from the medial margin of the carotid artery extending to the medial margin of the trapezius muscle (including levels II, III, IV, and V).
Each radiologist used uploaded CT data stored in the DICOM format in the fusion mode of the US system. The late postcontrast phase of the neck CT data was used. During scanning, a magnetic sensor installed on the tip of the probe sensed the magnetic field and detected the position and motion of the probe. At the beginning of image fusion, axial sections in the longest dimension of the most malignant-appearing thyroid nodule on the US and neck CT images were used. After this plane was registered, the presence of central LNM and lateral LNM were evaluated simultaneously.
Imaging Features of LNM on US and CT Images
The US criteria for LNM were as following: irregular cystic changes, microcalcifications, focal or diffuse hyperechogenicity, a length greater than 5 mm in short axis diameter with a round shape (long to short axial diameter ratio <1.5), and loss of fatty echogenic hilum [5-8]. In preoperative neck CT images, LNs were considered metastatic if any of the following criteria were met: central necrosis or cystic changes, dense cortical enhancement greater than that of muscle, or calcifications [3,9].
Statistical Analysis
The sensitivities, specificities, and diagnostic accuracies of the three modalities for detecting cervical LNM were calculated, using the final pathology report as the definitive standard. The McNemar test was performed to compare the sensitivity, specificity, and diagnostic accuracy of each imaging modality in the detection of central LNM and lateral LNM. All analyses were performed with PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA), and P-values of less than 0.05 were considered to indicate a statistically significant difference between modalities.
Results
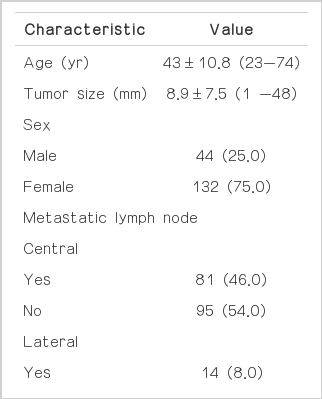
Among the 176 patients with PTC, 44 (25%) were male and 132 (75%) were female. The mean age and tumor size of all patients was 43 years (range, 23 to 74 years) and 8.9 mm (range, 1 to 48 mm), respectively. Demographic information about the patients is listed in Table 1. In the pathology reports, 81 patients were found to have central LNM, 14 patients were found to have lateral LNM, and 13 patients were determined to have both central and lateral LNM. All 176 patients underwent postoperative US and 14 patients with lateral LNM underwent a PET CT scan for evaluating local recurrence or distant metastasis, and the results of all exams were negative.
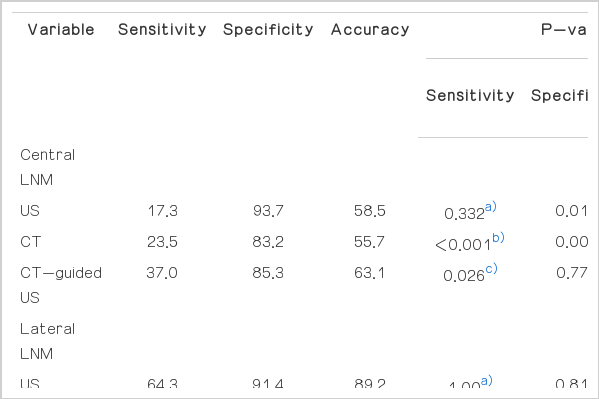
In the detection of central LNM, CT-guided US exhibited a significantly higher sensitivity (37.0%) compared to US (17.3%, P<0.001) and CT (23.5%, P=0.026). As well, the diagnostic accuracy of CT-guided US (63.1%) in detecting central LNM was higher than that of US (58.5%) and CT (55.7%), but these differences were not statistically significant. US showed a higher diagnostic accuracy (58.5%) in detecting central LNM than CT (55.7%, P=0.473) (Fig. 1), but it displayed a lower sensitivity (17.3%) than that of CT (23.5%, P=0.332). Therefore, some instances of deep-seated central LNM were detected only on the neck CT owing to the poor sonic window (Fig. 2). For the detection of lateral LNM, CT-guided US showed a higher sensitivity (92.9%) than that of US (64.3%, P=0.125) and CT (71.4%, P=0.375), although the differences were not statistically significant. The diagnostic accuracy of CT-guided US (96.0%) in detecting lateral LNM was significantly higher than that of US (89.2%, P=0.011) and CT (90.9%, P=0.063). CT showed better sensitivity (71.4%) with similar diagnostic accuracy for detecting lateral LNM than that of US (64.3%, P=1.00). Thus, some instances of lateral LNM were found on the neck CT and the CT-guided US, but not on US (Fig. 3). The sensitivities, specificities, diagnostic accuracies of US, neck CT, and CT-guided US are summarized in Table 2.
A 47-year-old woman with papillary thyroid cancer.
Ultrasonogram shows a hyperechoic lymph node (arrowheads) with loss of fatty echogenic hilum in the left neck level VI region. However, there is no demonstrable metastatic lymph node in the neck computed tomography. This lymph node was surgically confirmed as metastatic papillary carcinoma.

A 35-year-old woman with papillary thyroid cancer.
Neck computed tomography reveals that a suspicious lymph node (arrowheads) in the left neck level VI region, posterior to an ipsilateral malignant thyroid nodule (not shown), has a taller than wide shape with moderate enhancement. However, ultrasonogram did not show a definite metastatic lymph node. This lymph node was surgically confirmed as metastatic papillary carcinoma.
A 30-year-old woman with papillary thyroid cancer.
A. Neck computed tomography (CT) demonstrates two suspicious lymph nodes (arrowheads) with strong enhancement greater than that of adjacent muscle in the right level IV region of the neck. However, these lymph nodes were not found by ultrasonography (US). B. CT-guided US shows heterogeneous hyperechoic lymph nodes (arrowheads) with indistinct margins. This lymph node was surgically confirmed as metastatic papillary carcinoma.
Discussion
In thyroid cancer, preoperative imaging staging is a valuable tool for determining the extent of neck dissection. Several features that can be detected by US, such as the loss of hilar echogenicity, cystic necrosis, and calcifications, often indicate the presence of LNM [5-7]. US is better able than CT to characterize features of metastatic LN as small as 5 mm in diameter, due to its high-resolution images. However, US is unable to detect all instances of LNM, especially in the central compartment. In these circumstances, real-time neck CT-guided US would theoretically be able to overcome the disadvantages of US and improve diagnostic accuracy in areas with limited US visualization. It may also be useful for clinical decisionmaking when imaging discrepancies between US and neck CT occur regarding instances of suspicious LN.
In our study, US and neck CT exhibited high diagnostic accuracy in the detection of lateral LNM, a finding consistent with other published results [3,10,11]. To detect central LNM in preoperative US and CT-guided US images, we used a cut-off value of 5 mm for the short axis diameter. However, the sensitivities of these techniques were too low to use this cut-off as an indicator of central LNM. In our study, US and neck CT showed lower sensitivity and diagnostic accuracy for detecting central LNM compared with lateral LNM, a finding consistent with previous reports. However, our study found slightly lower values of sensitivity and diagnostic accuracy than those presented in previous reports regarding the detection of central LNM. One reason for this discrepancy may be the use of an adequately specific but not adequately sensitive cut-off value for LN size of 5 mm in diameter. Small LNs (less than 5 mm) often show many metastases; thus, we do not consider the size criterion alone to be acceptable for detecting central LNM. Furthermore, we included microscopic LNM along with whole LNM. Cumulatively, the size criterion used in this study, the presence of microscopic LNM may have led to lower sensitivity and diagnostic accuracy compared with other studies [3,10,11].
For lateral LNM, the metastasis criteria we used for preoperative US and neck CT exhibited reasonable accuracy compared with other results [3,10,11]. Among the 24 patients who underwent lateral LND in this study, lateral LNM was pathologically confirmed in 14 patients. We found that lateral LNM could be detected preoperatively by US and neck CT with approximately 68% sensitivity and 90% diagnostic accuracy, indicating that lateral LNM was more feasible to diagnose preoperatively than central LNM. This finding also indicates that latent LNM in the lateral compartment that is undetectable by US or neck CT remains undissected in a high proportion of patients. Our study demonstrated the overall superior sensitivity and diagnostic accuracy of CT-guided US for predicting central and lateral LNM compared with US or neck CT alone. Besides for predicting lateral LNM, CT-guided US showed higher sensitivity and diagnostic accuracy than combined US/CT without a fusion imaging system [3]. This means that CT-guided US is more useful than US or CT for making an accurate decision especially when suspicious LNM is found only on the neck CT, probably owing to the poor sonic window or the presence of imaging discrepancies between the US and the neck CT regarding a suspicious LN. Thus, we think that the above circumstances can be used as indications for CT-guided US.
Our study did have some limitations. First, during CT-guided US, point registration is subjective. Since no absolute reference points are available, each radiologist has to register the points individually by matching US and CT scans. Second, US can detect metastatic LN on a longitudinal or oblique scan. However, CT-guided US can only measure these parameters on a transverse scan; thus, discrepancies in LN size may occur. Third, we did not determine the inter-observer agreement on the readings of US, neck CT, and CT-guided US images. Fourth, we did not verify one-to-one correspondence between radiologically metastatic LN and pathologically confirmed metastatic LN. Fifth, our study was retrospective in its design. To fully evaluate the benefits of CT-guided US in the clinical setting, more prospective studies with objective measurements will be required.
In conclusion, according to the results of this study, CT-guided US of the neck may be a more accurate technique with higher sensitivity for detecting cervical LNM than either US or CT alone. Neck CTguided US might be useful in preoperative examinations, especially when there are areas with limited US visualization or when imaging discrepancies occur between conventional US and CT regarding a specific LN.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported in part by the Research Fund of the Korean Society of Ultrasound in Medicine.