Current status of automated breast ultrasonography
Article information
Abstract
Breast ultrasonography (US) is currently considered the first-line examination in the detection and characterization of breast lesions. However, conventional handheld US (HHUS) has several limitations such as operator dependence and the requirement of a considerable amount of radiologist time for whole-breast US. Automated breast US (ABUS), recently approved by the United States Food and Drug Administration for screening purposes, has several advantages over HHUS, such as higher reproducibility, less operator dependence, and less required physician time for image acquisition. In addition, ABUS provides both a coronal view and a relatively large field of view. Recent studies have reported that ABUS is promising in US screening for women with dense breasts and can potentially replace handheld second-look US in a preoperative setting.
Introduction
Mammography is an effective randomized controlled trial-proven method for reducing mortality due to breast cancer [1]. A recent study showed 43% reduction among women participating in a national screening program [2]. However, the sensitivity of mammography depends on breast density. Studies on women with dense breasts have demonstrated a sensitivity of less than 50% [3]. Asian women, including Korean women, have shown different mammographic densities. Approximately 70% of Korean women in their forties showed dense breasts, while only 46% of western women in their forties showed dense breasts [4,5]. More recently, more than 50% of women younger than 50 years and at least one-third aged over 50 years have been found to have dense breast tissue [6]. In addition, breast density has been established as an independent risk factor for breast cancer [7]. The current supplemental screening options include breast ultrasonography (US) and magnetic resonance imaging (MRI). US-based screening technologies may offer lower cost and wider availability than MRI. However, no clear guidelines have been established as to which modality to use for supplemental screening.
Handheld US (HHUS) is widely available and well tolerated. A large multicenter trial has demonstrated that screening with HHUS finds significantly more early-stage breast cancers than screening with mammography alone and has a cancer detection rate of 0.3%-0.5% [6,8-12]. However, bilateral whole-breast screening using HHUS is time consuming and has a high number of false positives. In addition, its practicability has been questioned because of the lack of standardized techniques, operator dependence, non-reproducibility, and time required by the radiologist to perform the exams [13]. Automated breast US (ABUS) was introduced more than a decade ago; at that time, the image quality of the scans was not sufficiently good to interpret the results. However, modern scanners of ABUS using high-frequency transducers have improved image quality. ABUS screening is an option proposed to overcome the time-consuming and costly nature of handheld, physician-performed whole-breast US (WBUS). However, there has been limited research on the applicability of ABUS because of the differences in the technique, data acquisition, and interpretation. In September 2012, the United States Food and Drug Administration (US FDA) approved an ABUS system (Somo-V ABUS, U-systems) to be used for whole-breast screening US after negative findings on mammography in women with dense breasts who have not previously undergone surgery or biopsy [14]. Recent breast density legislation in the United States has continued to increase the demand for supplemental US screening [15].
Equipment
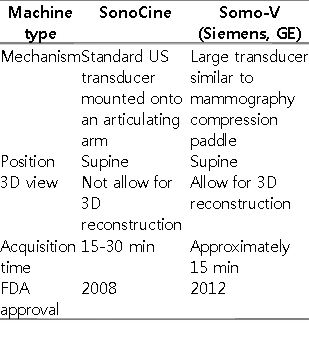
Traditionally, ABUS scanners have been classified as prone-type or supine-type scanners [16]. These scanners use various methods such as prone water-bath-type scanning and supine water-coupled scanning using 4- to 7-mHz transducers [16,17]. However, images obtained from old-generation automated scanners were of inferior quality to those generated by HHUS [18]. Recently, US manufacturers have been exploring automated WBUS methods to help streamline and standardize WBUS screening (Table 1). SonoCine Inc. has developed a hybrid system that combines a conventional high-resolution two-dimensional handheld transducer with an automated scanning arm to perform automated scanning [19]. A robotic device holds the HHUS transducer, which produces between 2,000 and 5,000 axial images of the screened area. This system received US FDA clearance in 2008. In this device, scanning is accomplished by mechanically moving the articulating arm over the breast in a way similar to that used for HHUS [20]. This technique does not allow for three-dimensional (3D) manipulation or reconstruction of the raw data. The imaging is reviewed in real time, in the same manner as any standard US examination would be reviewed, either at the time of examination or later if the examination were recorded and stored. Several studies using such an ABUS system have been published; the results of these studies were similar to those of studies conducted using HHUS for screening [19-21].
Another type of automated scanner is the one by Siemens AG and U-systems. This scanner is a standalone device and requires the patients to remain in a supine position. It uses a wide-field-of-view, large-footprint (15 cm×17 cm), high-frequency transducer and operates differently from HHUS (Fig. 1). Somo-V by U-systems was approved by the US FDA in 2012. It acquires raw data via a larger transducer similar in size and shape to a standard mammography compression paddle. The transducer paddle is placed over the breast, with a small amount of compression applied to stabilize the breast. Depending on the size of the breast, the US transducer plate might have to be repositioned and might require more than one scan to cover the breast. The average total time to complete the examination is 15 minutes. In our institution, we use Acuson S2000 ABVS (Siemens Medical Solutions, Mountain View, CA, USA), in which a typical exam consists of three automated 1-minute scans of each breast in the anterior-posterior position and both the oblique positions. Once the imaging data are obtained, they are processed using computer algorithms and stored on a hard drive. The images can then be reviewed on a standard workstation. During interpretation, images can be displayed in the transverse, coronal, or sagittal planes by using 3D data reconstruction (Fig. 2). Therefore, compared with HHUS, these systems do not provide additional clinical information such as that about a palpable lump or discharge because image acquisitions of this type of ABUS are performed by a technologist.
Acuson S2000 ABVS (automated breast volume scanner; Siemens Medical Solutions).
A, B. From the whole equipment (A), the transducer plate (B) is positioned over the breast and an automated scan is performed to obtain a series of two-dimensional images. Depending on the breast size, more than three scans per breast may be required.
A representative display of automated breast ultrasonography using Siemens ABVS.
Axial, sagittal, and coronal images were displayed together at a dedicated workstation. There is a probably benign mass in the right breast. The arrow indicates nipple marking.
Other types of automated US units in development utilize a scanning procedure that requires the patient to lie prone on the table. Scanning is performed in a rotational manner, with the transducer configured for circumferential data acquisition. The raw data are then processed and reconstructed to allow for 3D rendering [20].
Advantages of ABUS
ABUS has several advantages, compared with HHUS, irrespective of the type of ABUS system. First, ABUS is consistent and reproducible, while HHUS is operator dependent, meaning that the ability to detect and accurately document clinically significant findings in the case of HHUS is dependent upon the experience and expertise of the person performing the scanning [20]. Second, anyone can be trained to operate the ABUS equipment for scanning, while HHUS has to be conducted by a US technologist or a physician with the knowledge of US physics and anatomy. Third, the acquisition time of ABUS is more consistent. The total acquisition time averages 15 minutes for a patient with average-sized breasts and is slightly longer if more than the standard three views of each breast are needed in women with larger breasts. This consistent acquisition time can allocate an appropriate time slot for each patient, without unexpected delays, thus allowing a streamlined workflow. The physician time required by ABUS includes only the time required for interpretation, while the physician time required by HHUS includes the time required for performing the examination and that required for interpreting the results. When a radiologist becomes comfortable with reviewing and interpreting ABUS images, he/she would take approximately 3 minutes to read a negative examination. The time would increase to approximately 5 minutes when there are one or two significant findings. Occasionally, a case may still require 10 minutes or longer to fully interpret and report the results [20]. In addition, the coronal view is unique to ABUS; this view allows for a quick evaluation of the case and is useful in detecting the areas of architectural distortion. Fourth, the large probe of ABUS provides the whole coverage and characterization of the large mass (Fig. 3), and in the follow-up of large-sized cancer after neoadjuvant chemotherapy, it might provide an accurate measurement of a cancerous tumor larger than 5 cm.
Clinical Applications
ABUS in the Screening Setting
There are several studies comparing HHUS and ABUS. HHUS requires the time of a highly trained specialist to perform the examination (Table 2) [19,22-27]. The ACRIN 6666 study using a standard protocol may have extended the screening time beyond that required in normal practice [6,28]. Overall, 13-17 minutes is most likely the closest estimate of the time necessary to perform handheld WBUS. Thus, ABUS screening is an option proposed to overcome the time-consuming and costly nature of handheld, physician-performed WBUS, but there has been limited research on this topic [29].
Several studies have suggested that ABUS will play a promising role in the screening of women with dense breasts requiring mammography (Fig. 4). Kelly et al. [22] performed one multicenter prospective study comparing a combination of screening mammography and semiautomated WBUS with the individual methods alone in 4,419 women with dense breast tissue and/or at increased risk of breast cancer. The results of this study were promising, with an additional 3.6 cancers detected per 1,000 women screened, which is similar to the ACRIN 6666 results [6,19]. The sensitivity of the semiautomated WBUS alone was 67% (38/57) and that of mammography alone was 40% (23/57); however, the sensitivity of the combined modality was 81% (46/57) [19]. Kelly et al. [22] also evaluated the radiologist reader performance for cancer detection in women with dense breasts by using ABUS. They reported that the radiologists were able to improve cancer detection, with an increase of 63% in the callbacks of cancer cases and only a 4% decrease in the correct identification of true-negative cases [22]. In the ACRIN 6666 study evaluating HHUS screening, the authors described the following potential advantages of ABUS as a screening tool compared with HHUS: reduction of variability in examination performance, less operator dependence, and reduced physician time [6]. Golatta et al. [23] prospectively assessed a large number of 983 patients with 1,966 breasts. They reported a high negative predictive value of 98% (1,520/1,551), a high specificity of 85% (1,520/1,794), and a sensitivity of 74% (88/119), based on the cases of US-guided biopsy. Therefore, they suggested that ABUS might be a promising tool in breast imaging, particularly in screening settings [23]. Recently, two prospective multicenter studies evaluating the diagnostic performance of ABUS were conducted, and the results of these studies are expected to prove the value of ABUS as a screening tool and to validate ABUS’s equivalence to HHUS in terms of lesion detection [30,31].

A 40-year-old woman with an atypical papilloma identified by supplemental screening with automated breast ultrasonography (ABUS) in the left breast.
A. Mammography shows no definite abnormality in both breasts. B. ABUS shows a complex cystic mass in the left breast. Ultrasonography-guided core needle biopsy confirmed an atypical papilloma.
ABUS in the Diagnostic Setting
Several papers have reported the evaluation of the diagnostic performance of ABUS as a tool for preoperative evaluation, replacement of second-look US, and ductal carcinoma in situ (DCIS) evaluation [24-27,32-34]. However, the lesion detection, reliability, and interobserver concordance of ABUS need to be confirmed before the clinical application of ABUS in a diagnostic situation is considered [24,25,32,33]. Wenkel et al. [32] reported in their study of the diagnostic workup of clinical, mammographic, and sonographic abnormalities that all breast cancers were found using ABUS by all readers and correctly classified as Breast Imaging Reporting And Data System (BIRADS) 4 or 5, which showed good agreement regarding the BIRADS classification of HHUS and ABUS with kappa (k) values between 0.83 and 0.87. At that time Kotsianos-Hermle et al. [33], in their study on diagnostic workup, reported similar results, in which the sensitivity and the specificity of automated 3D US were comparable to those of manual US, but the coverage of the breast using ABUS was the main limitation. More recently, Shin et al. [24] reported the role of ABUS in a diagnostic setting in a preoperative evaluation of breast cancer (Fig. 5). In this study, ABUS reliably detected a lesion larger than 1.2 cm and exhibited high reliability in the reporting of lesion size and location in addition to substantial agreement on the description of the key feature and final assessment [24]. Recently, Wojcinski et al. [25] also reported a similar result with respect to the diagnostic performance and interobserver concordance of ABUS; they considered 100 ABUS scans in their study. They reported k values of 0.18 for the benign cases and 0.80 for the malignant cases. The combined assessments of readers 1 and 2 showed a diagnostic accuracy of 79%, sensitivity of 83%, and specificity of 78%. Xu et al. [34] evaluated the role of both ABUS and US elastography. They reported that both ABUS and US elastography showed substantial interobserver reliability and the combined use of ABUS and US elastography was useful in improving diagnostic accuracy and specificity [34].
A 44-year-old woman with multifocal cancers identified by preoperative automated breast ultrasonography (ABUS) in the right breast.
A. Mammography shows an irregular isodense mass in the right lower breast (arrow). B. Coronal view of ABUS shows two irregular hypoechoic masses in the lower inner quadrant of the right breast (arrows), which were assessed as multifocal malignancies. Right breast conserving surgery confirmed two invasive ductal carcinomas.
As for the preoperative assessment of pure DCIS, Li et al. [26] performed a prospective study consisting of 33 patients with pure DCIS. They reported that ABUS showed a better correlation with the extent of disease of pure DCIS than HHUS (64% for ABUS vs. 42% for HHUS) and could provide more accurate information preoperatively. In addition, Chae et al. [27] assessed the role of ABUS as a replacement for handheld second-look US (HH-SLUS), in which three radiologists evaluated 80 additional suspicious lesions detected on preoperative breast MRI. They described in their study that 8 of the 15 lesions (53%) that were not detected on HH-SLUS, were detected on ABUS. Therefore, they concluded that ABUS might help in deciding upon a biopsy guidance method as a replacement tool for HH-SLUS [27].
Lastly, it is important to develop techniques to help radiologists to reduce the reading time and to minimize the number of unnecessary recalls, by aiding them to distinguish between benign and malignant lesions [35]. A computer-aided diagnosis (CAD) system can help readers to assess the probability that a certain lesion is malignant [35,36]. Tan et al. [35] reported that without extensive training, the use of the CAD system improves the performance of less-experienced readers in distinguishing malignant from benign lesions in ABUS.
Summary
In summary, ABUS is a promising new technology that might be useful for screening for breast cancer in women with dense breast tissue; it has recently been approved by the US FDA for screening use. ABUS can potentially help in the preoperative evaluation of breast cancer, including pure DCIS, and may replace HH-SLUS in a preoperative evaluation for the detection of suspicious lesions detected on breast MRI. Therefore, ABUS is expected to become a preferred option for enabling widespread use of US screening and for replacing HH-SLUS in a preoperative setting.
Notes
No potential conflict of interest relevant to this article was reported.