AbstractPurposeThis study was conducted to evaluate the prevalence of perineal trauma during childbirth and to assess the correlations of the pelvic floor dimensions and fetal head station with obstetric trauma in a prospectively recruited cohort of women.
MethodsThe study included women with a gestational age of at least 37 weeks, who were carrying a single fetus in a cephalic presentation. Transperineal ultrasound (TPU) was performed prior to the onset of labor or labor induction. The purpose was to measure the anteroposterior diameter (APD) of the levator ani muscle (LAM) and the angle of progression, at both rest and maximum Valsalva maneuver. The head-perineum distance was assessed only at rest.
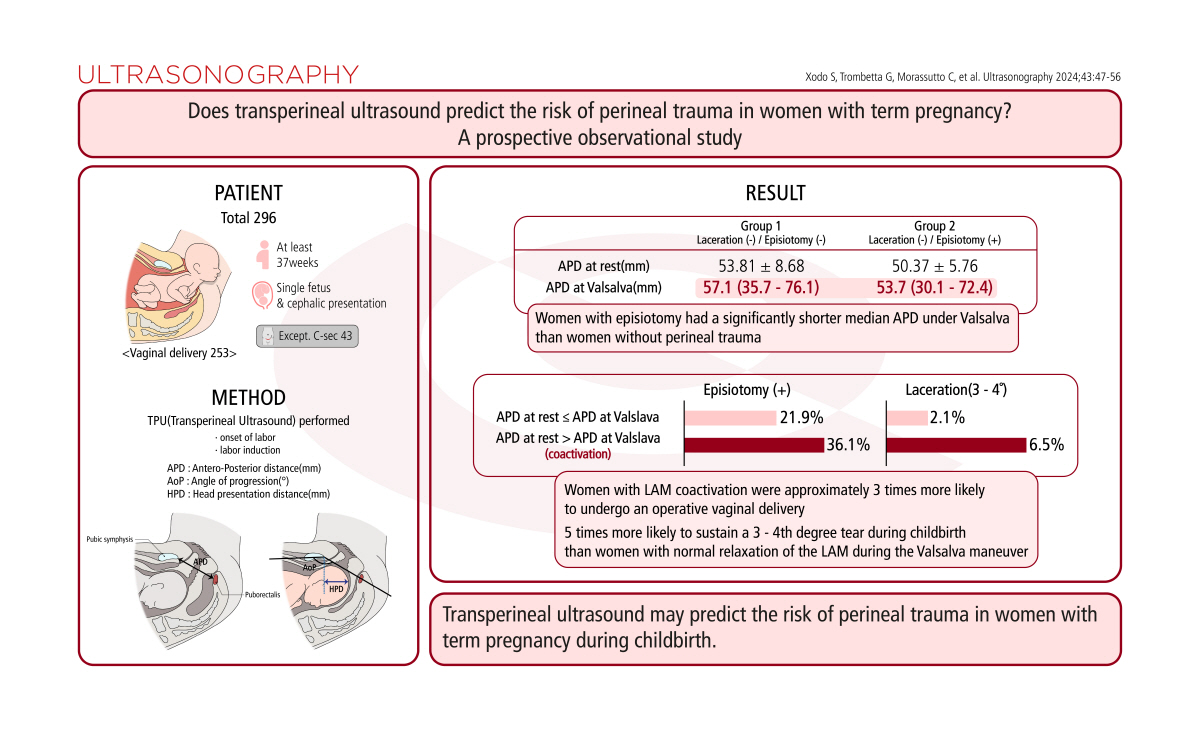
ResultsA total of 296 women were included. Of the 253 women who delivered vaginally, 19% (48/253) experienced no perineal trauma, 18.2% (46/253) received an episiotomy during childbirth, 34.4% (87/253) sustained a first-degree laceration, 25.3% (64/253) had a second-degree laceration, and 3.2% had a third- or fourth-degree laceration (8/253). Women with episiotomy had a significantly shorter median APD under Valsalva than women without perineal trauma. Furthermore, women with LAM coactivation (identified by a negative difference between the APD at Valsalva and the APD at rest) were approximately three times more likely to undergo an operative vaginal delivery and over five times more likely to sustain a third- or fourth-degree tear during childbirth than women who exhibited normal relaxation of the LAM during the Valsalva maneuver.
Perineal trauma is a relatively common occurrence during childbirth. Most women experience some form of laceration during vaginal delivery, with the majority classified as first- or second-degree lacerations [1]. More severe perineal lacerations, which extend through the anal sphincter complex, are known as obstetric anal sphincter injuries (OASIS) [1]. Episiotomy, a surgical procedure that enlarges the posterior aspect of the vagina via an incision to the perineum, may be performed during the final part of the second stage of labor. While midline episiotomy is the most common type in the United States, mediolateral episiotomy is more frequently performed in Europe. Perineal trauma during childbirth can lead to both short-term and long-term complications, including bleeding, infection, urinary and fecal incontinence, and dyspareunia [2]. The frequency of perineal trauma varies based on factors such as patient characteristics, birth setting, and practices of the care provider. A meta-analysis of 22 studies identified the strongest risk factors for OASIS as operative vaginal delivery, midline episiotomy, and increased fetal birth weight. Other risk factors that showed significant associations with severe perineal trauma included primiparity, Asian ethnicity, labor induction, labor augmentation, epidural anesthesia, and persistent occiput posterior position [3].
Transperineal ultrasound (TPU) has gained popularity as a tool for assessing the pelvic floor [4]. This approach has enhanced understanding of the labor mechanism, particularly with respect to the levator ani muscle (LAM), the primary component of the pelvic floor. Several studies have shown a strong correlation between successful vaginal delivery and LAM relaxation during maternal pushing. Conversely, failure of vaginal delivery is associated with coactivation, defined as muscle contraction during the Valsalva maneuver [5,6]. However, the impact of coactivation on perineal trauma in women undergoing vaginal delivery has not been previously evaluated.
The primary objective of this study was to assess the prevalence of perineal trauma within a prospectively recruited cohort of women while distinguishing between various types of trauma, given that women may concurrently experience multiple forms of perineal injuries. The secondary aim was to evaluate the relationships of the pelvic floor dimensions and the fetal head station, both at rest and during the Valsalva maneuver prior to the onset of labor, with obstetric trauma, including spontaneous obstetric laceration and/or episiotomy.
Ethical approval was obtained (CEUR-2019-Os-26). Informed consent was obtained from all individuals included in this study.
This study was a prospective observational investigation, conducted from February to December 2022 at the Clinic of Obstetrics and Gynecology of the University Hospital of Udine. Recruitment was focused on women at term of gestation (that is, beyond 37+0 weeks of gestation), who had singleton pregnancies with the fetus in cephalic presentation.
The exclusion criteria encompassed the following: women who had undergone prior uterine surgery, women who were in active labor or exhibited membrane rupture at the time of enrollment, and fetuses with an estimated weight above the 95th percentile (as determined by the Hadlock formula) [7].
At the time of enrollment, all anthropometric and anamnestic data related to the women were collected. These included age, parity, body mass index (BMI), obstetric history, and (for multiparous women) any previous perineal lacerations or episiotomies. Following this initial data collection, and prior to the spontaneous onset of labor or admission for labor induction, a TPU procedure was conducted. This was performed using a convex transducer covered by a glove (Philips Affiniti 70/Voluson E8; GE Healthcare, Chicago, IL, USA). The procedures were carried out by two operators (GT and GB), each with more than 5 years of experience.
The TPU was performed with the patient in the dorsal resting position following bladder emptying. A mid-sagittal view was acquired, which displayed the following anatomical landmarks: the pubic symphysis, bladder, fetal head, vagina, rectum, and puborectalis muscle. From this view, two measurements were taken: the anteroposterior diameter (APD) of the LAM [6] and the angle of progression (AoP) [8]. The APD was measured at the shortest distance between the posteroinferior border of the pubic symphysis and the anterior border of the puborectalis muscle. The AoP is defined as the angle formed by a straight line drawn along the longitudinal axis of the pubic bone and a line drawn from the inferior edge of the pubic bone to the leading edge of the fetal cranium.
The APD and AoP were measured both at rest and under maximum Valsalva maneuver. By rotating the transducer 90┬░ clockwise in a resting state, an axial plane was subsequently established. On this plane, an additional parameter, the head-perineum distance (HPD), was assessed [9]. The HPD was determined as the shortest distance from the outer bony limit of the fetal skull to the skin surface of the perineum (Fig. 1).
The birth attendants, including both the midwife and the delivery physicians, were blinded to the TPU measurements. The second stage of labor was characterized as the period from full cervical dilation to delivery. The maximum duration of the second stage of labor aligned with the local protocol, which adhered to the Society for Maternal-Fetal Medicine guidelines: a maximum of 3 hours for nulliparous women (or up to 4 hours with epidural analgesia) and 2 hours for multiparous women (or up to 3 hours with epidural analgesia) [10]. Episiotomies were carried out by midwives, based on their subjective clinical judgement. In the hospital at which this study took place, episiotomies were consistently performed in a mediolateral manner. The procedure involved making an incision 4 cm long and 3 cm deep, positioned at a 45┬░ angle on the right side of the vulva, within 1 cm of the posterior commissure of the vaginal orifice. This incision was made when the tissues were stretched by the babyŌĆÖs head [11]. The vaginal opening was enlarged by an episiotomy when conditions necessitated a shortening of the second stage of labor. Such conditions included maternal exhaustion, a non-reassuring fetal heart rate, the need for vacuum instrumentation, shoulder dystocia, and anticipation of a severe perineal tear. Furthermore, birth attendants employed maneuvers to safeguard the perineum during the second stage of labor [12].
The following data were gathered regarding labor and delivery: induction of labor, application of epidural analgesia, interval from analgesia to delivery, duration of the first and second stages of labor, and mode of delivery (spontaneous, vacuum-assisted, or cesarean). Additional data included whether an episiotomy was performed and/or the degree of perineal laceration, the neonateŌĆÖs weight and sex, the Apgar score, the arterial pH of the umbilical cord, the volume of blood loss, the weight of the placenta, and the results of histological examination.
The primary endpoint of the study was computed by calculating the ratio of women with each type of perineal tear, including episiotomy, to the total number of women recruited. Each calculated value was accompanied by its corresponding confidence interval (CI). Based on the assumption that the prevalence of perineal tears of the second degree or higher was 26% in this population, and with an acceptable error margin of 5%, it was necessary to recruit 296 women for the study to achieve clinical significance [13,14].
Continuous distributions are represented as the mean (┬▒standard deviation) for parametric data and as the median and interquartile range for non-parametric data. Categorical data are expressed as absolute values and percentages. The results of logistic regression are displayed as odds ratios (ORs) with 95% CIs.
The study population was categorized into five groups based on the presence or absence of perineal trauma, as well as the specific type of perineal trauma experienced. To compare these groups, the Friedman analysis of variance or the Kruskal-Wallis test was utilized, followed by the Dunn post hoc test.
The sample was subsequently divided into two groups according to whether an episiotomy was present or absent, and then further categorized based on the presence or absence of LAM coactivation during maximum Valsalva maneuver. The indices measured in the groups were compared using either the Student unpaired two-tailed t-test or the Mann-Whitney U test. The chi-square test was employed for the comparison of frequencies. Both univariable and multivariable logistic regression analyses were conducted to evaluate the factors potentially associated with episiotomy and operative vaginal deliveries. However, for third- or fourth-degree perineal tears, only univariate logistic regression was performed due to the limited number of events.
Statistical analyses were conducted using SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA), with P-values of less than 0.05 considered to indicate statistical significance.
The analysis included a total of 296 women. Table 1 presents the maternal characteristics and labor outcomes. Of the population studied, 218 patients (73.7%) experienced a spontaneous vaginal delivery, 35 (11.8%) underwent an operative vaginal delivery, and 43 (14.5%) had a cesarean delivery. Among the 253 women who delivered vaginally, 19% (48/253) did not sustain any perineal trauma, 18.2% (46/253) received an episiotomy during childbirth, 34.4% (87/253) experienced a first-degree laceration, 25.3% (64/253) had a second-degree laceration, and 3.2% (8/253) had a third- or fourth-degree laceration. Table 2 provides the baseline characteristics, TPU measurements, and obstetric outcomes of the participants, categorized into five groups based on the type of perineal trauma experienced during childbirth.
Women who underwent an episiotomy exhibited a significantly shorter median APD under the Valsalva maneuver compared to women who did not experience perineal trauma. The group of women with OASIS, the most severe type of spontaneous obstetric laceration, displayed the shortest median APD value. Furthermore, the OASIS group demonstrated a negative difference between the median APD under Valsalva maneuver and the median APD at rest.
Women with OASIS, those who received an episiotomy, and those with a second-degree obstetric laceration experienced a significantly longer duration of the second stage of labor compared to women with an intact perineum or a first-degree obstetric laceration. Logistic regression analysis revealed that the risk of episiotomy decreased as the APD value under the Valsalva maneuver increased. The only independent variable that made a significant contribution to the model was APD under the Valsalva maneuver, with an OR of 0.956 (95% CI, 0.928 to 0.986; P<0.05). This significant contribution was also observed in the multivariate model (OR, 0.964; 95% CI, 0.934 to 0.995; P<0.05), even after adjusting for factors such as maternal age, pre-pregnancy BMI, neonatal weight, analgesia, and oxytocin induction/augmentation.
Table 3 presents the baseline characteristics, TPU measurements, and obstetric outcomes of the participants, with the women divided into two groups based on whether they exhibited LAM coactivation. This was determined by a negative difference between the APD at Valsalva and the APD at rest [15]. The data revealed that women with LAM coactivation more frequently required operative vaginal delivery and episiotomy compared to those without LAM coactivation. Additionally, the second stage of labor was significantly longer in women with LAM coactivation than in those without it. The logistic regression analysis demonstrated that women with LAM coactivation were over five times more likely to experience a third- or fourth-degree tear during childbirth (OR, 5.857; 95% CI, 1.181 to 29.040; P<0.05) compared to women who exhibited normal LAM relaxation during the Valsalva maneuver. The logistic regression analysis also showed that women with LAM coactivation were over three times more likely to undergo an operative vaginal delivery (OR, 3.238; 95% CI, 1.543 to 6.797; P<0.05). Even after adjusting for factors such as maternal age, pre-pregnancy BMI, neonatal weight, analgesia, and oxytocin induction/augmentation, this risk remained significant (OR, 2.643; 95% CI, 1.221 to 5.724; P<0.05).
This study revealed that 25.29% of women received an episiotomy, while 28.45% experienced an obstetric laceration of the second degree or higher. Additionally, women who had an episiotomy demonstrated shorter levator hiatus diameters under the Valsalva maneuver, as assessed at term of gestation prior to the onset of labor via TPU. In a comparison between women with normal LAM function and those with coactivation of this muscle during the Valsalva maneuver, the latter group were found to experience a longer second stage of labor. They also more frequently required an episiotomy and were at an approximately threefold elevated risk of operative vaginal delivery. Moreover, they faced greater than a fivefold higher risk of sustaining a third- or fourth-degree tear during childbirth.
Episiotomy is a surgical incision of the vagina and perineum, performed by an experienced birth attendant to enlarge the vaginal opening [16]. Following the publication of evidence for restricting the use of episiotomy, the global rates of this procedure have generally decreased. However, substantial disparities remain among countries, with rates as low as 9.7% in Sweden and as high as 100% in Taiwan and Guatemala [17]. In this study, the prevalence of episiotomy was approximately 25%, lower than the 59.2% rate reported previously [11]. The present value is slightly higher than the overall rate in Italy, which is around 20% [18]. The reduction in episiotomy rates at the institute of the present study reflects the adherence to recommendations advocating for the selective use of episiotomy. However, recent research has explored the role of episiotomy in instrumental vaginal deliveries as a potential protective factor for the perineum. According to the most recent systematic review and meta-analysis, which included more than 700,000 patients, mediolateral or lateral episiotomy was found to reduce the rate of OASIS in instrumental vaginal deliveries, whether with ventouse or forceps [19]. Furthermore, some authors have found a positive correlation between episiotomy and improved neonatal condition at birth in cases of medically assisted vaginal delivery [20]. Interestingly, the World Health Organization noted in 2018 that determining an "acceptable" rate of episiotomy is challenging, indicating that subjective clinical judgment remains the key determining factor [21]. Before performing an episiotomy, the birth attendant should weigh the potential benefits, such as facilitating delivery for maternal or fetal indications, against the potential adverse effects of the procedure. These may include the extension of injury leading to third- and fourth-degree perineal tears [3,22], increased rates of infection, other anatomical complications such as fistula or narrowing of the introitus, and increased blood loss [23].
Another key finding of the present study is that approximately one in four women experienced a second-degree perineal tear. This type of perineal tear is receiving increased scrutiny in the literature, as recent studies have indicated that it can negatively affect womenŌĆÖs daily lives, including their sexual function, even beyond the initial 6 months postpartum [24-26]. Furthermore, the present study revealed an OASIS rate of approximately 3%, a figure that closely aligns with the frequency reported in England [27]. The most serious concern regarding OASIS is that this type of injury heightens the risk of subsequent loss of bowel control [28-31].
Given that the etiologies of pelvic floor disorders are frequently linked to pregnancy and childbirth, the prevention of episiotomy and OASIS is a desirable outcome related to childbirth. A recent systematic review and meta-analysis of prospective cohort studies identified a range of risk factors for these disorders. For urinary incontinence, these factors included urinary incontinence during pregnancy, instrumental vaginal delivery, episiotomy, tears, and constipation. Meanwhile, risk factors for fecal incontinence included fecal incontinence during pregnancy, maternal age over 35 years, prenatal BMI greater than 30 kg/m2, instrumental vaginal delivery, spontaneous vaginal delivery, oxytocin augmentation, and birth weight exceeding 4,000 g [32]. The present study is the first to demonstrate that TPU conducted before the onset of labor can be used to identify women at elevated risk of requiring an episiotomy during childbirth. Specifically, this study found that these women had a significantly shorter LAM APD during the Valsalva maneuver. The final part of the second stage of labor, which involves the passage of the fetal head, is characterized by hyperdistention of the urogenital hiatus. This is enabled by adequate LAM relaxation during maternal pushing [4]. This finding could be noteworthy, as these women might benefit from pelvic training cycles targeting LAM function, even during pregnancy.
The other two ultrasound parameters that reflect the head station, namely the HPD and the AoP, were found to not be significantly associated with adverse obstetric outcomes when measured prior to labor. This finding may suggest that the HPD and AoP become more important during labor, particularly when analyzing the curves of fetal head descent in relation to the mode of delivery and the remaining duration of labor [33].
The LAM is a fan-shaped layer of striated muscle that plays a crucial role in defining vaginal anatomy and function. It forms a V-or U-shaped sling, with arms extending from each pelvic sidewall towards the posterior aspect of the anorectal junction. This muscle engages in various physiological functions during the Valsalva maneuver, a process involving forced expiration with a closed glottis, which results in a marked increase in intra-abdominal pressure. Depending on the physiological function required, the LAM can contract (for instance, to maintain continence), or relax in situations such as defecation, voiding, or vaginal birth [6]. In 2007, Orno and Dietz characterized LAM coactivation as when the distance between the inferoposterior rim of the symphysis pubis and the pubovisceral muscle component of the LAM during the Valsalva maneuver is less than that in the resting state. That study, which was part of broader research on pelvic floor function and anatomy during pregnancy, revealed that women with LAM coactivation had significantly lower bladder neck descent than women without coactivation [15]. More recently, Youssef et al. [4] investigated the correlation between LAM coactivation and labor outcomes. They found that LAM coactivation detected before labor was associated with an increased duration of the second stage of labor [34-36] and a higher fetal head station [37,38]. The present study is the first to evaluate the correlation between LAM coactivation at term pregnancy before labor and perineal trauma during vaginal birth. The findings align with the existing literature, confirming that women with LAM coactivation experience a longer second stage of labor [34-36]. Moreover, the data indicate that the most severe types of perineal trauma related to childbirth, namely episiotomy and OASIS, occur more frequently in women with LAM coactivation. Specifically, logistic regression analysis revealed that women who could not adequately relax the LAM during the Valsalva maneuver had more than five times the risk of experiencing a third- or fourth-degree perineal tear (OR, 5.857; 95% CI, 1.181 to 29.040) relative to women who could relax this muscle.
The present study revealed that women who co-contract the LAM during Valsalva are over three times more likely to require an operative vaginal delivery, with an OR of 3.238 (95% CI, 1.543 to 6.797). This finding deviates slightly from what is suggested in the literature. Multiple studies have indeed indicated that women with larger levator hiatal dimensions are relatively likely to have a spontaneous vaginal delivery [6,39]. Furthermore, Van Veelen et al. [5] demonstrated that smaller levator hiatal dimensions during pelvic floor contraction in a first pregnancy were associated with subsequent instrumental vaginal delivery or cesarean delivery due to failure to progress. However, the present data diverge from this focus on pelvic biometry, instead considering the coactivation of the LAM. This approach illuminates the impact of this phenomenon on the need for medical intervention during vaginal delivery.
The primary clinical implication of this study is that TPU may assist clinicians in identifying women with term pregnancy who are at elevated risk of requiring an episiotomy or developing severe spontaneous perineal trauma during childbirth. This information is highly relevant, as various techniques can be employed during labor to mitigate the risk of perineal trauma, including perineal massage [40], hands-on methods [41,42], and warm compresses [41]. However, even more intriguing is the potential to direct high-risk women (identified via antenatal TPU) towards pelvic floor interventions, such as pelvic floor muscle training and/or perineal massage, during pregnancy. It would then be possible to evaluate whether the clinical situation has improved by repeating the TPU following the pelvic floor intervention program. Moreover, if future studies corroborate these findings, clinicians should provide adequate counseling to women about the potential complications that can arise from vaginal delivery.
Recent interest in the coactivation of the LAM among researchers suggests a need for future studies focused on teaching women to relax this muscle during the Valsalva maneuver. New research has highlighted the importance of visual biofeedback as a tool that can enhance self-regulation in women. In a pilot study, laboring women who received epidural analgesia and visual biofeedback using TPU showed improved pushing efficacy, which led to a reduced incidence of perineal tearing. In that study, the authors clearly demonstrated to patients how the measured AoP, which reflects the descent of the head, changed during their pushing efforts. This suggests that the training process could benefit from active patient involvement [43]. This approach could be applied in future studies with the objective of increasing women's awareness of their pelvic floor muscles, particularly the LAM.
The present authors posit that pelvic training could potentially enhance labor outcomes for women who do not adequately relax the LAM during childbirth.
This study is the first to evaluate the potential utility of TPU performed prior to the onset of labor in predicting severe perineal lacerations, including episiotomy. Previous research has shown a strong association between LAM coactivation and a longer second stage of labor [34-36]. The present study not only corroborates this finding but also reports an increased probability of women with LAM co-contraction under Valsalva, assessed during the antenatal period, undergoing an operative vaginal delivery and developing OASIS. Another strength of the present study is the blinding of birth attendants to the TPU measurements. This approach prevented the potential influence of knowledge about the received intervention on the outcome measure. Furthermore, the increased levels of risk among women with LAM coactivation of operative vaginal delivery and severe perineal tear during childbirth were confirmed by multivariate logistic regression analysis. This analysis accounted for variables such as maternal age, pre-pregnancy BMI, neonatal weight, analgesia, and oxytocin use.
Several limitations in this study warrant discussion. First, the second stage of labor was not subdivided into the passive phase, which spans from full cervical dilation to the onset of active pushing, and the active second stage, defined as the period from active pushing to the delivery of the infant. As a result, the impact of LAM coactivation on the expulsive stage may have been biased. Second, additional measurements such as those of the urogenital area and the transverse diameter could have provided more specific insights into perineal properties. However, these ultrasonographic parameters are challenging to acquire and often require highly skilled operators. A third potential limitation pertains to the timing of the TPU. In this study, the decision was made to conduct the perineal assessment in the final weeks preceding delivery. It could, however, be fruitful to perform this scan earlier, providing ample time to attempt correction of the LAM coactivation through appropriate perineal training.
In summary, the present study demonstrates that women who require an episiotomy during childbirth typically have a shorter APD, as assessed through TPU prior to the onset of labor. Furthermore, inadequate relaxation of the pelvic floor muscles during antenatal Valsalva maneuvers is associated with an approximately threefold increase in the risk of requiring an instrumental vaginal delivery, and more than a fivefold increase in the risk of developing a third- or fourth-degree perineal tear.
NotesAuthor Contributions Conceptualization: Xodo S, Trombetta G, Morassutto C, Londero AP. Data acquisition: Xodo S, Trombetta G, Baccarini G, Celante L, Driul L. Data analysis or interpretation: Morassutto C, Londero AP. Drafting of the manuscript: Xodo S, Londero AP. Critical revision of the manuscript: Xodo S, Trombetta G, Morassutto C, Baccarini G, Celante L, Driul L, Londero AP. Approval of the final version of the manuscript: all authors. References1. Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 198: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol 2018;132:e87ŌĆōe102.
2. Abedzadeh-Kalahroudi M, Talebian A, Sadat Z, Mesdaghinia E. Perineal trauma: incidence and its risk factors. J Obstet Gynaecol 2019;39:206ŌĆō211.
3. Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G. Risk factors for severe perineal lacerations during childbirth. Int J Gynaecol Obstet 2014;125:6ŌĆō14.
4. Youssef A, Brunelli E, Pilu G, Dietz HP. The maternal pelvic floor and labor outcome. Am J Obstet Gynecol MFM 2021;3:100452.
5. van Veelen GA, Schweitzer KJ, van Hoogenhuijze NE, van der Vaart CH. Association between levator hiatal dimensions on ultrasound during first pregnancy and mode of delivery. Ultrasound Obstet Gynecol 2015;45:333ŌĆō338.
6. Lanzarone V, Dietz HP. Three-dimensional ultrasound imaging of the levator hiatus in late pregnancy and associations with delivery outcomes. Aust N Z J Obstet Gynaecol 2007;47:176ŌĆō180.
7. Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body, and femur measurements: a prospective study. Am J Obstet Gynecol 1985;151:333ŌĆō337.
8. Barbera AF, Pombar X, Perugino G, Lezotte DC, Hobbins JC. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet Gynecol 2009;33:313ŌĆō319.
9. Eggebo TM, Gjessing LK, Heien C, Smedvig E, Okland I, Romundstad P, et al. Prediction of labor and delivery by transperineal ultrasound in pregnancies with prelabor rupture of membranes at term. Ultrasound Obstet Gynecol 2006;27:387ŌĆō391.
10. Obstetric care consensus no. 1: safe prevention of the primary
cesarean delivery. Obstet Gynecol 2014;123:693ŌĆō711.
11. Bertozzi S, Londero AP, Fruscalzo A, Driul L, Delneri C, Calcagno A, et al. Impact of episiotomy on pelvic floor disorders and their influence on women's wellness after the sixth month postpartum: a retrospective study. BMC Womens Health 2011;11:12.
12. The OASI Care Bundle [Internet]. London: Royal College of Obstetricians and Gynaecologists, 2023. [cited 2023 Aug 30]. Available from: https://www.rcog.org.uk/about-us/quality-improvement-clinical-audit-and-research-projects/oasi/OASI care bunlde.
13. Arya R, Antonisamy B, Kumar S. Sample size estimation in prevalence studies. Indian J Pediatr 2012;79:1482ŌĆō1488.
14. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench 2013;6:14ŌĆō17.
15. Orno AK, Dietz HP. Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol 2007;30:346ŌĆō350.
16. Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev 2017;2:CD000081.
17. Graham ID, Carroli G, Davies C, Medves JM. Episiotomy rates around the world: an update. Birth 2005;32:219ŌĆō223.
18. Mencancini C, Maraschini A, Giordani B, Seccareccia F, Davoli M, Donati S, et al. Perinatal health in Italy: data from the National Outcomes Program (years 2015-2020). Boll Epidemiol Naz 2022;3:38ŌĆō45.
19. Okeahialam NA, Wong KW, Jha S, Sultan AH, Thakar R. Mediolateral/lateral episiotomy with operative vaginal delivery and the risk reduction of obstetric anal sphincter injury (OASI): a systematic review and meta-analysis. Int Urogynecol J 2022;33:1393ŌĆō1405.
20. Desplanches T, Marchand-Martin L, Szczepanski ED, Ruillier M, Cottenet J, Semama D, et al. Mediolateral episiotomy and risk of obstetric anal sphincter injuries and adverse neonatal outcomes during operative vaginal delivery in nulliparous women: a propensity-score analysis. BMC Pregnancy Childbirth 2022;22:48.
21. Intrapartum care for a positive childbirth experience [Internet]. Geneva: World Health Organization, 2017. [cited 2023 Aug 30]. Available from: https://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/en/.
22. Pergialiotis V, Bellos I, Fanaki M, Vrachnis N, Doumouchtsis SK. Risk factors for severe perineal trauma during childbirth: an updated meta-analysis. Eur J Obstet Gynecol Reprod Biol 2020;247:94ŌĆō100.
23. Macleod M, Strachan B, Bahl R, Howarth L, Goyder K, Van de Venne M, et al. A prospective cohort study of maternal and neonatal morbidity in relation to use of episiotomy at operative vaginal delivery. BJOG 2008;115:1688ŌĆō1694.
24. Leeman L, Rogers R, Borders N, Teaf D, Qualls C. The effect of perineal lacerations on pelvic floor function and anatomy at 6 months postpartum in a prospective cohort of nulliparous women. Birth 2016;43:293ŌĆō302.
25. Lindberg I, Persson M, Nilsson M, Uustal E, Lindqvist M. "Taken by surprise" - Women's experiences of the first eight weeks after a second degree perineal tear at childbirth. Midwifery 2020;87:102748.
26. Macedo MD, Ellstrom Engh M, Siafarikas F. Detailed classification of second-degree perineal tears in the delivery ward: an inter-rater agreement study. Acta Obstet Gynecol Scand 2022;101:880ŌĆō888.
27. Green-Top Guideline No. 29. The management of third- and fourth-degree perineal tears. London: Royal College of Obstetricians and Gynaecologists, 2015.
28. Richter HE, Nager CW, Burgio KL, Whitworth R, Weidner AC, Schaffer J, et al. Incidence and predictors of anal incontinence after obstetric anal sphincter injury in primiparous women. Female Pelvic Med Reconstr Surg 2015;21:182ŌĆō189.
29. Andrews V, Shelmeridine S, Sultan AH, Thakar R. Anal and urinary incontinence 4 years after a vaginal delivery. Int Urogynecol J 2013;24:55ŌĆō60.
30. Sangalli MR, Floris L, Faltin D, Weil A. Anal incontinence in women with third or fourth degree perineal tears and subsequent vaginal deliveries. Aust N Z J Obstet Gynaecol 2000;40:244ŌĆō248.
31. Gommesen D, Nohr EA, Qvist N, Rasch V. Obstetric perineal ruptures-risk of anal incontinence among primiparous women 12 months postpartum: a prospective cohort study. Am J Obstet Gynecol 2020;222:165.
32. Hage-Fransen MA, Wiezer M, Otto A, Wieffer-Platvoet MS, Slotman MH, Nijhuis-van der Sanden MW, et al. Pregnancy- and obstetric-related risk factors for urinary incontinence, fecal incontinence, or pelvic organ prolapse later in life: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2021;100:373ŌĆō382.
33. Hjartardottir H, Lund SH, Benediktsdottir S, Geirsson RT, Eggebo TM. Fetal descent in nulliparous women assessed by ultrasound: a longitudinal study. Am J Obstet Gynecol 2021;224:378.
34. Kamel R, Montaguti E, Nicolaides KH, Soliman M, Dodaro MG, Negm S, et al. Contraction of the levator ani muscle during Valsalva maneuver (coactivation) is associated with a longer active second stage of labor in nulliparous women undergoing induction of labor. Am J Obstet Gynecol 2019;220:189.
35. Brunelli E, Del Prete B, Casadio P, Pilu G, Youssef A. The dynamic change of the anteroposterior diameter of the levator hiatus under Valsalva maneuver at term and labor outcome. Neurourol Urodyn 2020;39:2353ŌĆō2360.
36. Youssef A, Montaguti E, Dodaro MG, Kamel R, Rizzo N, Pilu G. Levator ani muscle coactivation at term is associated with longer second stage of labor in nulliparous women. Ultrasound Obstet Gynecol 2019;53:686ŌĆō692.
37. Youssef A, Brunelli E, Montaguti E, Di Donna G, Dodaro MG, Bianchini L, et al. Transperineal ultrasound assessment of maternal pelvic floor at term and fetal head engagement. Ultrasound Obstet Gynecol 2020;56:921ŌĆō927.
38. Youssef A, Brunelli E, Fiorentini M, Pilu G, El-Balat A. The correlation between levator ani co-activation and fetal head regression on maternal pushing at term. J Matern Fetal Neonatal Med 2022;35:9654ŌĆō9660.
39. Siafarikas F, Staer-Jensen J, Hilde G, Bo K, Ellstrom Engh M. Levator hiatus dimensions in late pregnancy and the process of labor: a 3- and 4-dimensional transperineal ultrasound study. Am J Obstet Gynecol 2014;210:484.
40. Aquino CI, Guida M, Saccone G, Cruz Y, Vitagliano A, Zullo F, et al. Perineal massage during labor: a systematic review and meta-analysis of randomized controlled trials. J Matern Fetal Neonatal Med 2020;33:1051ŌĆō1063.
41. Aasheim V, Nilsen AB, Reinar LM, Lukasse M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 2017;6:CD006672.
Mid-sagittal view (A-D) and axial view (E) acquired through trans-perineal ultrasound with empty bladder and dorsal resting position.A. The levator ani anteroposterior diameter (APD) was measured at rest and it is 51.2 mm. B. The levator ani APD was measured under the maximum Valsalva maneuver, and it is 64.2 mm. C. The angle of progression (AoP) was measured at rest and it is 103.9┬░. D. The AoP was measured under the maximum Valsalva maneuver and it is 115┬░. E. The head-perineum distance was measured at rest and it is 36.6 mm. PB, pubic symphysis; UB, urinary bladder; VAG, vagina; R, rectum; A, anus; PR, puborectalis muscle.
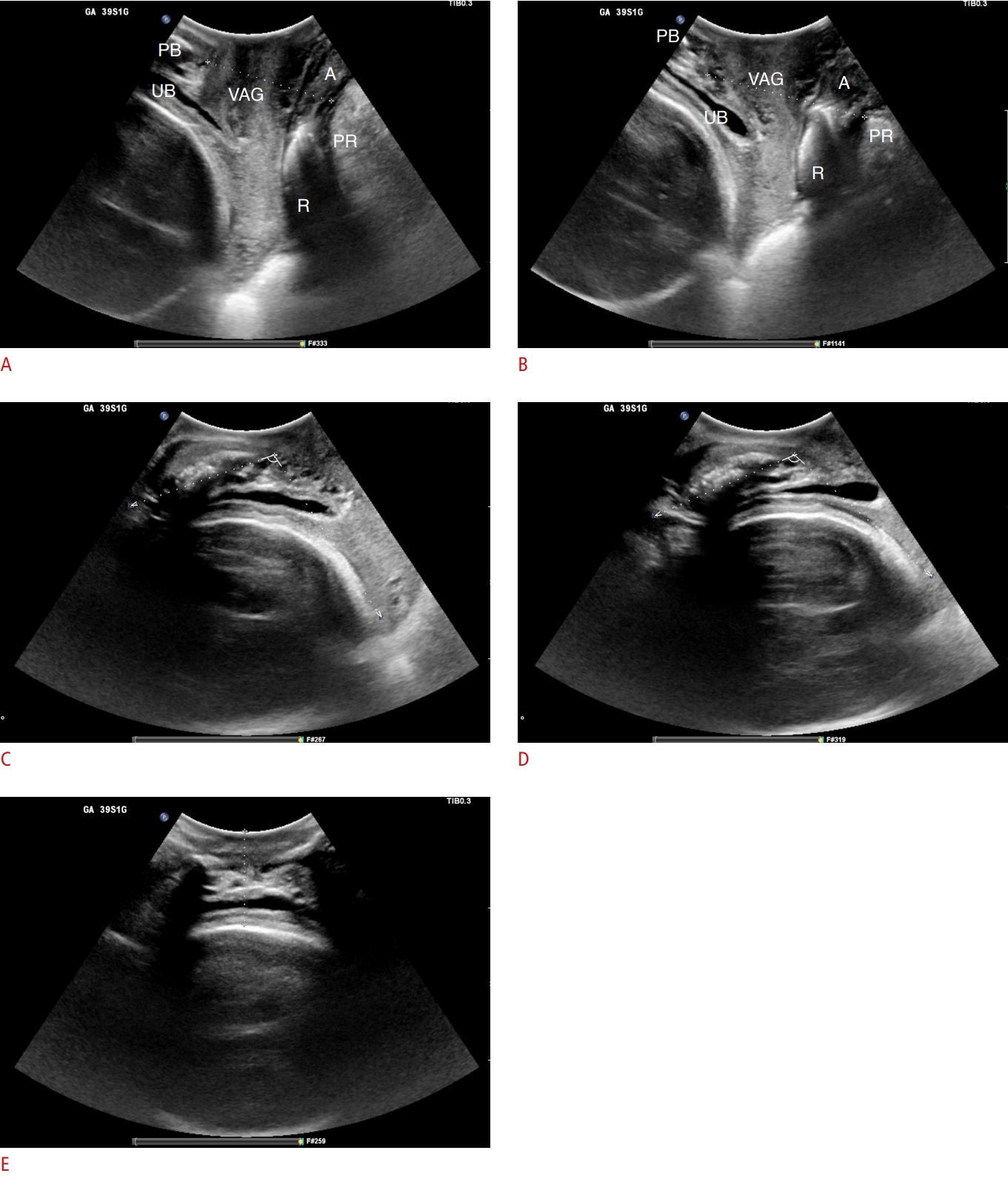 Fig.┬Ā1.Table┬Ā1.Demographic and clinical characteristics of women included in the study (296 women) Table┬Ā2.Comparison of five groups (253 women) according to the presence or absence and type of perineal trauma
Values are presented as number (%), mean┬▒SD, or median (min-max). Lac0epi0, intact perineum; Lac0epi1, episiotomy (no lacerations); Lac1, first-degree perineal tear; Lac2, second-degree perineal tear; Lac3 or 4, third- or fourth-degree perineal tear; SD, standard deviation; BMI, body mass index; APD, anteroposterior diameter of levator ani muscle; AoP, angle of progression; HPD, head-perineum distance. Table┬Ā3.Comparison between two groups (296 women) according to the presence or absence of levator ani muscle coactivation
Values are presented as mean┬▒SD, median (min-max), or number (%). APD, anteroposterior diameter of levator ani muscle; BMI, body mass index; AoP, angle of progression; HPD, head-perineum distance; Lac0epi0, intact perineum; Lac0epi1, episiotomy (no lacerations); Lac1, first-degree perineal tear; Lac2, second-degree perineal tear; Lac3 or 4, third- or fourth-degree perineal tear. |



 Print
Print facebook
facebook twitter
twitter Linkedin
Linkedin google+
google+
 Download Citation
Download Citation PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI




