AbstractPurposeThe objective of this study was to evaluate pain and image quality associated with the use of two different ultrasound transducers.
MethodsFifty healthy male participants aged 30 years or older were prospectively enrolled. All ultrasound procedures were performed using a V8 machine (Samsung Medison, Seoul, Korea) equipped with EA2-11 (conventional) and miniER7 (small-caliber) transrectal transducers, operated by a single genitourinary radiologist. To minimize bias, one group of volunteers underwent ultrasonography with the conventional transducer first, followed by the small transducer. For the remaining participants, the examinations were performed in the opposite order. Ultrasonography, including the measurement of total prostate and transitional zone volumes, was conducted in accordance with standard practice. After testing with both probes, participants were asked to rate their pain on a 10-point numerical rating scale (NRS). A radiologist then evaluated the quality of the images acquired with each probe using a 5-point numeric scale and compared the prostate volume measurements obtained by each method.
ResultsThe mean NRS scores associated with the conventional and small transducers were 4.7±1.8 and 2.7±1.2, respectively (P<0.05). The mean ultrasound image qualities from the two transducers were statistically similar (4.78 and 4.74, P>0.05). The whole prostate gland volume as measured with the conventional transducer (mean±standard deviation, 24.2±9.1 mL) was greater than the measurement (22.1±8.7 mL) obtained with the small-caliber transducer (P<0.05). However, only two of the 50 whole gland volume measurements differed by more than two standard deviations.
IntroductionProstate ultrasonography is an essential diagnostic instrument for evaluating prostate diseases. This non-invasive, relatively affordable, and widely available imaging modality assists in the diagnosis and monitoring of various prostate conditions. These include the detection and localization of prostate abnormalities, biopsy guidance, cancer staging, treatment planning and monitoring, assessment of post-treatment complications, and evaluation of lower urinary tract symptoms.
Conventional transrectal ultrasonography (TRUS) transducers are commonly used in prostate ultrasonography due to their capacity to produce detailed images. The use of such devices is now considered a standard method for prostate ultrasonography [1,2]. Generally, this procedure is viewed as convenient and tolerable. However, the insertion of these transducers often causes discomfort and pain for certain patients, presenting a challenge for both the patients and the medical professionals involved [3]. The primary sources of this pain are believed to be the forceful stretching of an unrelaxed anal sphincter and the direct contact of the ultrasound transducer [4]. Pain during insertion can be exacerbated by increased anal tone in younger patients and local inflammatory conditions such as anal fissures or fistulas. This discomfort can result in patient anxiety and reluctance to undergo necessary diagnostic procedures, potentially delaying the detection and treatment of prostate diseases. Moreover, the discomfort experienced during prostate ultrasonography can hinder medical professionals in obtaining clear images, which could potentially impact the accuracy of the diagnosis.
In response to these clinical challenges, researchers have focused on the development of a small-caliber transrectal transducer. The goal is to minimize patient discomfort while maintaining comparable image quality to conventional transducers [5]. The small-caliber transducer is designed to be less invasive, thereby providing a more comfortable experience for patients undergoing prostate ultrasonography. However, regarding image quality, the use of a smaller probe carries a risk of diminished resolution or penetration. This article explores whether examinations conducted with smaller transrectal probes can offer a more comfortable, less invasive alternative to conventional transducers while maintaining adequate image quality.
Materials and MethodsCompliance with Ethical StandardsInstitutional review board approval was granted for this prospective interventional study (Seoul National University Bundang Hospital IRB No. B-2207-771-305), and informed consent was obtained from all participants.
Participant EnrollmentThe study was a single-arm, prospective experimental investigation conducted at an academic tertiary referral hospital in South Korea. It is registered with the Clinical Research Information Service [https://cris.nih.go.kr]; registration number: KCT0008247.
Between October 2022 and February 2023, we enrolled 50 healthy male volunteers aged 30 years or older. Participants were excluded from the study if they met any of the following criteria: (1) inability to undergo transrectal ultrasound due to anal obstruction, such as among patients who had undergone colon cancer surgery, (2) inability to tolerate the pain associated with the insertion of the ultrasound probe due to anal narrowing, and (3) a recent history of prostatitis or transurethral prostatectomy. Given the experimental nature of this human study and the lack of previous data, no sample size estimation was performed.
Experimental DesignTRUS was conducted using a Samsung Medison V8 device (Samsung Medison, Seoul, Korea) with a standard transrectal transducer (EA2- 11AR) and a small-caliber transducer (MiniER7). The procedure was performed by a board-certified genitourinary radiologist with 19 years of experience. The cut surface areas of the standard and small transducer were 385 mm2 and 222 mm2, respectively. In a single session, a volunteer underwent multiple examinations using both the standard and small-caliber transducers. To minimize bias resulting from the order of transducer insertion, for half of the 50 participants, the conventional transducer was used first, followed by the small-bore transducer. For those remaining, the order was reversed. The patients were blinded to the types of transducers used during each examination session. All measurements during TRUS were taken by a single radiologist. The transverse and anteroposterior diameters were measured in the axial plane, while the longitudinal diameter was measured in the midsagittal plane. Separate diameter measurements were taken for the whole gland and the transition zone. The volumes of the whole gland and transition zone were automatically calculated using the ellipsoid prolate formula (transverse diameter×anterior-posterior diameter×longitudinal diameter×0.523). A routine TRUS examination, including color Doppler ultrasound, was performed with each transducer.
Study OutcomesThe primary outcome of this study was the pain or discomfort experienced by participants during the ultrasound examination. This pain was assessed at the end of the procedure conducted using each transducer, either conventional or small-caliber. At the time of consent, all participants were instructed to quantify their pain using a numeric rating scale (NRS), which ranged from 0 (indicating no pain) to 10 (indicating the worst possible pain). Two NRS scores, one from the standard transducer and one from the small-caliber transducer, were recorded for each patient and subsequently compared.
The secondary outcomes of this study included the image quality and the measurement of prostate volume acquired with each transducer. The image quality was evaluated by another genitourinary radiologist with 19 years of experience. The criteria for image quality included: (1) a clear margin of the entire prostate gland; (2) no focal acoustic shadowing; (3) no ultrasonic artifacts; and (4) adequate image resolution for the internal architecture. If all criteria were met, the ultrasound image received a rating of 5. The score was reduced by the number of unfulfilled criteria. For instance, if one criterion was not met, a score of 4 was assigned, constituting a 1-point deduction from 5. The volumes of the whole prostate gland and the transition zone, measured with each transducer, were compared.
Statistical AnalysisThe pain score as rated using the NRS, image quality, and prostate volumetry using the standard and small-caliber transducers were compared using the paired t-test. A Bland-Altman plot was constructed to illustrate the relationship between the differences and the magnitude of each volume measurement. Pearson correlation analysis was conducted to determine the correlations of the volumes measured with each probe. All statistical analyses were carried out using MedCalc 20.218 (MedCalc, Mariakerke, Ostend, Belgium).
ResultsThe mean age of the 50 volunteers enrolled was 43 years (range, 31 to 73 years). None of the volunteers were excluded based on the eligibility criteria. The mean NRS±the standard deviation (SD) values for the conventional and small-caliber transducers were 4.7±1.8 (range, 1 to 8) and 2.7±1.2 (range, 1 to 5), respectively (P<0.05) (Fig. 1). No significant differences in NRS were observed between the first insertion (3.9±2.0) and the second (3.5±1.6) (P>0.05). The mean±SD of image quality was 4.78±0.4 for the conventional transducer and 4.74±0.4 for the smaller-caliber transducer (P>0.05) (Fig. 2). The mean ultrasound image qualities from the two transducers were statistically similar.
The mean±SD volume of the whole prostate gland was 24.2±9.1 mL (range, 11.4 to 63.8 mL) when measured with the conventional transducer. In contrast, it was 22.1±8.7 mL (range, 10.4 to 60.2 mL) when measured using the small-caliber transducer (P<0.05). However, for the transition zone volume, the conventional transducer recorded a smaller mean volume (5.8±3.9 mL) than the small-caliber transducer (6.2±4.2 mL) (P<0.05). Bland-Altman plots of both the whole gland volume and the transition zone volume revealed that 48 and 47 of 50 measurements, respectively, fell within two standard deviations, indicating no systematic variation between the two measurement methods (Fig. 3). Both measurements also demonstrated high correlations, with Pearson correlation coefficients of 0.9662 for the whole gland volume and 0.9677 for the transition zone volume (P<0.05) (Fig. 4).
DiscussionThe findings of this study indicate that the small-caliber transducer significantly lowered pain scores, as measured by the NRS, compared to the conventional transducer. This suggests that the small-caliber transducer provides a more comfortable and less invasive alternative for patients undergoing prostate ultrasonography, thereby addressing the discomfort and anxiety frequently associated with the procedure. The mean NRS for the conventional transducer in this study was 4.7, which is slightly higher than the mean NRS reported by Hou et al. [3]. This discrepancy can primarily be attributed to the younger mean age (43 years) of the participants in this study compared to those in the Hou et al.'s study [3] (mean age, 63 years). It is well-documented that anorectal compliance is lower and resting anal tone is relatively higher in younger patients during the insertion and withdrawal of the transducer [6,7].
No significant difference in image quality was found between the two transducers, suggesting that the small-caliber transducer can provide diagnostic information comparable to that of the conventional transducer. This supports the potential clinical use of small-caliber transducers, as they can maintain adequate image quality while providing a more comfortable and less invasive experience for patients undergoing prostate ultrasonography. The factors affecting the images due to the reduction in probe size included decreased penetration and lateral resolution. Although the penetration was at 83% of the level of conventional products, it could still cover the 6-cm depth required for prostate diagnosis. Given the size of the prostate, we believe that this would be sufficient for most patients, even those with prostate hyperplasia. The fields of view of the conventional probe and the miniER7 were similar, at 150° and 146°, respectively. The line density was also comparable, as the scan lines set in the image are similar in number and not sparse. The decrease in resolution increased as the depth increased, but the effect was not significant up to 6 cm, resulting in little difference in the images produced by the miniER7. However, in deeper areas, the transmission and reception aperture narrows, reducing the lateral resolution to approximately 80% relative to the traditional probe. Within 6 cm, the far field image quality was similar, regardless of the center frequency.
Another aim of this study was to compare the volume measurements of the whole prostate gland and transition zone obtained using the conventional and small-caliber transrectal probes. Statistically significant differences were observed in the mean volumes measured by the two transducers, with the smaller probe tending to yield smaller measurements for the whole volume. The transverse and longitudinal lengths of the prostate, as measured by the smaller transducer, were typically smaller than those measured with the conventional transducer. Conversely, the anterior-posterior lengths of the prostate were larger (Fig. 2). It can be inferred that the smaller-caliber transrectal probe causes less stretching of the prostate gland. The Pearson correlation coefficients for both the whole gland and transition zone volume measurements showed high correlations between the probes. Additionally, Bland-Altman plots revealed no systematic variation between the measurements. Jeong et al. [8] found that the mean volume measured by TRUS was larger than the actual prostate volume post-proctectomy. The ultrasound transducer used in that study was an end-firing transrectal ultrasound (5 to 9 MHz) in the HDI 5000 (Philips Medical Systems, Best, The Netherlands), with a diameter similar to that of the conventional transducer used herein. These findings suggest that the small-caliber transducer can provide reliable and accurate volume measurements of the prostate gland, positioning it as a viable alternative to conventional transducers in clinical practice.
TRUS may cause patients discomfort and, occasionally, pain. Although infrequent, rectal bleeding can occur due to injuries induced by the transducer. However, these instances are so rare that no substantial references are available. More often, rectal bleeding complications are associated with transrectal-guided prostate biopsies rather than ultrasound procedures. At the authors’ affiliated institution, approximately 5,000 TRUS examinations are performed each year. Reports of rectal bleeding are only received once every two to three years, typically from patients with pre-existing conditions such as hemorrhoids or a history of anal fissures. The presence of hemorrhoids can significantly increase pain during TRUS [3]. The true prevalence of hemorrhoids is uncertain, but self-reported incidence rates are 4.4% of the population in the United States [9], 11% in certain European Union countries [10], and 14.4% in Korea [11]. Particularly when considering the increase in caliber due to the device attached to the transducer during a TRUS-guided biopsy, it is thought that using a smaller-caliber transducer may result in greater pain reduction.
The limitations of this study were as follows. First, this study was based on healthy volunteers, so the results may differ slightly in older male patients with enlarged prostates due to hyperplasia [12]. However, given that pain during TRUS is positively correlated with prostate volume [3], the pain-reducing effect of a smaller probe could be greater in older patients. Second, although we blinded the participants to the order of transducer insertion, they were aware that different types of transducers would be used. This may have triggered a psychological tendency to perceive one as less painful than the other. Third, the image quality analysis was focused on the general imaging features of TRUS. The evaluation did not include significant focal lesions in the prostate, such as cancer, because the study was based on healthy volunteers. However, given that the characteristics of the ultrasonograms produced by the two different transducers were quite similar, minimal differences are expected in the detection or characterization of any type of lesion.
In conclusion, the small-caliber transducer provides a less invasive and more comfortable alternative to the traditional transrectal probe used in prostate ultrasonography, without sacrificing image quality. Its broad clinical application could substantially improve patient experience and compliance with essential diagnostic procedures for prostate diseases.
NotesAuthor Contributions Conceptualization: Hwang SI. Data acquisition: Hwang SI. Data analysis or interpretation: Hwang SI, Ahn H, Lee HJ, Jung SI. Drafting of the manuscript: Hwang SI. Critical revision of the manuscript: Hwang SI, Ahn H, Lee HJ, Jung SI. Approval of the final version of the manuscript: all authors. Conflict of InterestSung Il Hwang is presently the recipient of a research grant from Samsung Medison Co., Ltd. The funder had no role in the design of the study; the collection, analyses, or interpretation of the data; the writing of the manuscript, or the decision to publish the results. The remaining authors declare no conflicts of interest. References1. Mitterberger M, Horninger W, Aigner F, Pinggera GM, Steppan I, Rehder P, et al. Ultrasound of the prostate. Cancer Imaging 2010;10:40–48.
2. Hwang SI, Lee HJ. The future perspectives in transrectal prostate ultrasound guided biopsy. Prostate Int 2014;2:153–160.
3. Hou CP, Lin YH, Hsieh MC, Chen CL, Chang PL, Huang YC, et al. Identifying the variables associated with pain during transrectal ultrasonography of the prostate. Patient Prefer Adherence 2015;9:1207–1212.
4. Nazir B. Pain during transrectal ultrasound-guided prostate biopsy and the role of periprostatic nerve block: what radiologists should know. Korean J Radiol 2014;15:543–553.
5. Ghai S, Toi A. Role of transrectal ultrasonography in prostate cancer. Radiol Clin North Am 2012;50:1061–1073.
6. Philip J, McCabe JE, Roy SD, Samsudin A, Campbell IM, Javle P. Site of local anaesthesia in transrectal ultrasonography-guided 12-core prostate biopsy: does it make a difference? BJU Int 2006;97:263–265.
7. Rodriguez A, Kyriakou G, Leray E, Lobel B, Guille F. Prospective study comparing two methods of anaesthesia for prostate biopsies: apex periprostatic nerve block versus intrarectal lidocaine gel: review of the literature. Eur Urol 2003;44:195–200.
8. Jeong CW, Park HK, Hong SK, Byun SS, Lee HJ, Lee SE. Comparison of prostate volume measured by transrectal ultrasonography and MRI with the actual prostate volume measured after radical prostatectomy. Urol Int 2008;81:179–185.
9. Sun Z, Migaly J. Review of hemorrhoid disease: presentation and management. Clin Colon Rectal Surg 2016;29:22–29.
10. Sheikh P, Regnier C, Goron F, Salmat G. The prevalence, characteristics and treatment of hemorrhoidal disease: results of an international web-based survey. J Comp Eff Res 2020;9:1219–1232.
Box-and-whisker plot illustrating the mean numeric rating scale of pain (NRS) values obtained with the conventional transducer (Co) and the small-caliber transducer (Small).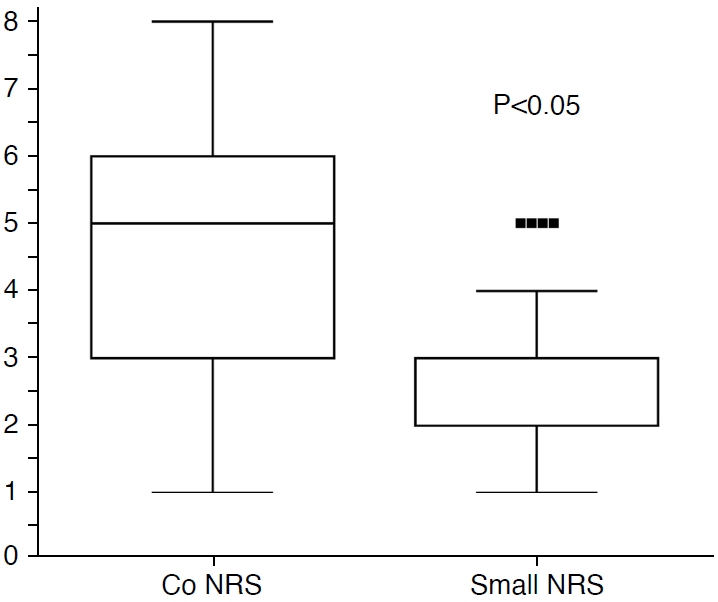 Fig. 1.Transverse gray-scale transrectal ultrasonography image taken utilizing a conventional transducer (A) and a small-caliber transducer (B).The boundaries of the prostate gland are clearly defined. No focal acoustic shadowing or ultrasonic artifacts are evident. The surgical capsule of the transition zone (indicated by arrows) is similarly visible in both images. Note the variations in the deformed posterior margin of the prostate (arrowheads) caused by the different calibers of the transducers.
 Fig. 2.Bland-Altman plots of the whole gland volume (A) and the transition zone volume (B).For (A), two of the 50 measurements fell outside of two standard deviations (SDs), while for (B), three of the 50 measurements did so. Co-TOV, total volume measured by conventional transducer; Small-TOV, total volume measured by small transducer; Co-TZV, transition zone volume measured by conventional transducer; Small-TZV, transition zone volume measured by small transducer.
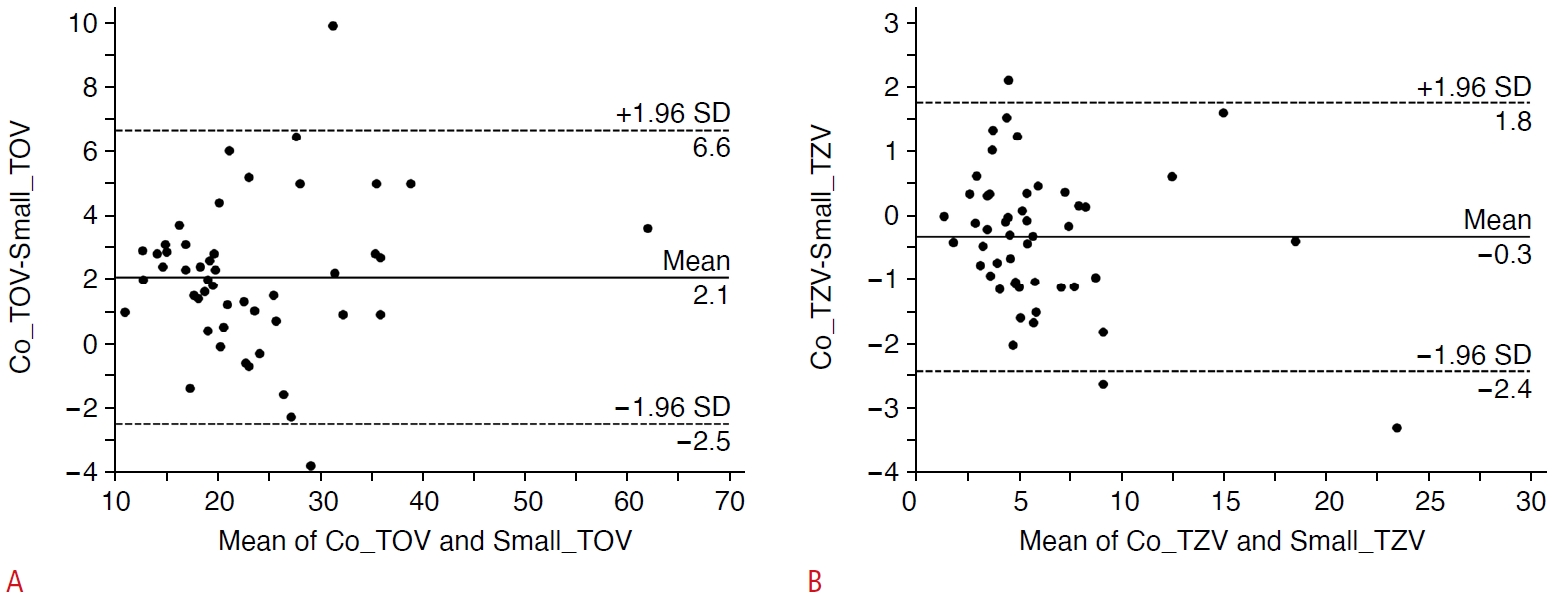 Fig. 3.Scatter plot used to calculate Pearson correlation coefficients for measurement of the whole gland volume (A) and the transition zone volume (B).A high correlation was noted between the values obtained using the two transducer types. Co-TOV, total volume measured by conventional transducer; Small-TOV, total volume measured by small transducer; Co-TZV, transition zone volume measured by conventional transducer; Small-TZV, transition zone volume measured by small transducer.
 Fig. 4. |